Coronary heart disease is the second cause of death in Chilean women, with higher mortality among women, especially at younger ages. The objective was to analyze in-hospital case-fatality by sex and age in patients with acute myocardial infarction in Chile and to evaluate associated factors.
MethodsFrom the nationwide hospital admissions database and the GEMI registry (a multicenter registry), we selected all cases of acute myocardial infarction (code: I.21) that occurred between 2001 and 2007 in Chile. We estimated odds ratios for in-hospital case-fatality in women by age (crude and adjusted for clinical characteristics and treatment).
ResultsIn total, 49 287 cases of acute myocardial infarction were hospitalized, 31.3% of them women; 9278 patients were incorporated in the GEMI registry (27.1% women). In-hospital case-fatality was higher (P<.001) in women than men (national database, 20.4% vs 11.3%; GEMI, 14.2% vs 7.3%, irrespective of age. In-hospital case-fatality risk was higher in women aged<45 years: national odds ratio=2.3 (95% confidence interval, 1.5-3.3) and GEMI, odds ratio=2.7 (1.1-6.8). The estimated risk was lower in women aged 75 or more years in both databases, 1.3 (1.2-2.4) and 1.5 (1.2-1.9), respectively. Younger women less often received statins, odds ratio=0.7 (0.6-0.8); acetylsalicylic acid, odds ratio=0.4 (0.2-0.6); betablockers, odds ratio=0.8 (0.6-0.9), and thrombolytics, odds ratio=0.6 (0.5-0.8). An interaction was found between Killip class and sex. After adjusting for covariates, women aged<55 years with ST-segment elevation myocardial infarction and Killip class I-II, had the highest risk, odds ratio=4.3 (2.1-8.9).
ConclusionsIn the context of a Latin American country, women aged<55 years with ST-segment elevation myocardial infarction and Killip class I-II had a higher risk of death. Known risk factors do not completely explain this excess of risk.
Keywords
.
IntroductionCardiovascular diseases are the main cause of death in the adult population in Chile, particularly cerebrovascular disease and coronary artery disease. Among Chilean women aged 45 years and older, these 2 diseases are the leading cause of death.1
Higher in-hospital mortality rates among women is widely documented in international and Chilean registries.2–9 The excess risk might be explained by delayed diagnosis, the lower use of therapies indicated in clinical guidelines, older age at the time of acute myocardial infarction (AMI), and the higher prevalence of risk factors among women.2,3,10–13 In Chile, data from the Multicenter Study Group on Infarction (GEMI) registry show that women undergo fewer reperfusion and revascularization procedures than men and also receive fewer drugs of proven pharmacological efficacy.6 This treatment gap narrowed after AMI was included in the universal health plan (Regimen of Explicit Health Guarantees), which since 2005 has guaranteed medical care for patients with AMI from diagnosis through to secondary prevention in the entire population, regardless of their health insurance.4 The results from the GEMI registry are in agreement with international studies published after the guidelines were implemented.5 However, in-hospital mortality is still twice as high among women as among men. It has been reported that this excess risk is even greater among younger women compared with men in the same age range.14–17
The objective of the present study was to analyze the in-hospital mortality according to sex and age of patients with AMI in Chile, which can be considered as a model Latin American country with medium-high income.18 In addition, possible explanations were explored. The working hypothesis was that younger women are at greater risk of in-hospital death due to AMI compared to men of the same age, even after adjusting for clinical factors.
MethodsStudy Design and PopulationFor the present study, all cases of AMI (ICD code, 10 I.21) reported between 2001 and 2007 in the national database for hospital admissions and in the GEMI hospital registry over the same period were selected.
Data Sources and CollectionThe nationwide hospital database records information on all admissions to hospital, whether public or private, in Chile. The data is digitalized by trained staff, and then processed by the Department of Health Statistics and Information of the Chilean Health Ministry. Information on diagnosis, sex, age at the time of infarction, condition on discharge, and type of hospital (public or private) was collected from this database. In Chile, healthcare institutions are classified as public or private: public establishments provide care to those with least resources and receive a subsidy from the state. This variable was therefore used as a proxy measure of socioeconomic level.
The GEMI registry was designed as a prospective, multicenter registry of patients with diagnosis of AMI with or without ST elevation, admitted to public or private hospitals in the different regions of Chile. The patients included in the registry have elevated creatine kinase and an MB fraction twice or more the normal value or troponin elevation above the normal value. They also must have at least one of the following criteria: a) typical chest pain lasting at least 30min, and b) abnormal electrocardiogram characteristic of AMI (ST elevation or depression≥0.1mV at 2 or more adjacent leads, pathologic Q waves, or new left bundle branch block). The registry began collecting data in 1993 and has incorporated patients continuously through to the present day. Participation by the hospitals is voluntary, and so this is a convenience sample of patients who, for the most part, come from bigger hospitals, many of which are reference hospitals in their respective regions. In each case, a form is completed that collects information on demographic and socioeconomic characteristics, medical history, treatment, and outcome of hospitalization. The information is then digitalized and processed in a central facility of the Chilean Society of Cardiology and Cardiovascular Surgery.
Thus, the GEMI database is a sample of the cases of AMI registered in Chile, and provides additional information that is not included in other national databases.
In the study period, 9909 patients from 29 centers with different catchment populations were included in the GEMI registry. Of this total, 55 patients with no information on sex or age were excluded (n=9854). Subsequently, reference hospitals for their respective regions or health areas with a constant participation in the registry (at least 5 of the 7 years studied) were selected. The final sample was therefore reduced to 16 centers and 9278 patients (94% of the initial sample).
Statistical AnalysisAn exploratory analysis of the data was undertaken, checking the normal distribution of the continuous variables with the Shapiro-Wilk test. Quantitative variables were described as means (standard deviation) or quartiles, depending on their distribution, and qualitative variables as absolute and relative frequencies.
In-hospital mortality was calculated, defined as the ratio of deaths due to AMI during hospitalization and total of cases diagnosed and hospitalized with AMI. Mortality was calculated by sex and age group, divided into 10-year intervals from<45 years to≥75 years. To compare these variables according to group and between databases, the Student t test or the Wilcoxon test were used for continuous variables, the χ2 test for categorical variables. In addition, the trend towards in-hospital mortality in the different age groups was assessed using the χ2 trend test.
The odds ratios (ORs) were estimated along with the 95% confidence interval (CI95%), both raw and adjusted for socioeconomic status, for in-hospital mortality of women at a national level and in the GEMI registry for the different age groups (taking men as reference). From the information in the GEMI registry, multiple logistic regression models were constructed to estimate the risk of in-hospital mortality in women, stratified according to type of infarction (with and without ST elevation) and age group. The models were adjusted by risk factors (diabetes mellitus, hypertension, dyslipidemia, obesity, and tobacco use), prior infarction, Killip functional class on admission (Killip I and II vs III and IV), treatments during hospitalization (beta blockers, angiotensin-converting enzyme inhibitors, acetylsalicylic acid, and statins), and reperfusion procedures (primary angioplasty and thrombolysis). To achieve groups of comparable size, only 4 age groups were used:<55, 55-64, 65-74, and≥75 years. In total, 353 patients were excluded because they did not have a diagnostic electrocardiogram, 239 because there was no electrocardiographic information, and 360 for the absence of information on Killip class on admission. The final sample for the multivariate model was composed of 8464 patients, 91.2% of the initial sample. To assess the impact of these losses on the estimates, a sensitivity analysis was done taking the best possible case for the Killip variable. The final model included only those variables that showed a statistically significant association in the univariate analysis. After each model, the predictive capacity was assessed by calculating the specificity and sensitivity for providing the correct classification. The STATA 11.219 statistical package was used and statistical significance set to 5%.
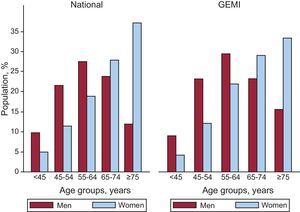
ResultsAnalysis of Mortality According to Age and SexIn Chile, 49 287 patients were admitted to hospital for AMI between 2001 and 2007. Of these, 31.3% (n=15 408) were women, with a mean age of 68.6 (13.6) years, whereas the mean age of men was 61.5 (13.2) years (P<.001). In the GEMI registry, in the same period, 9278 patients were included, with women accounting for 27.1% (n=2517). The mean age of women was 67.8 (12.7) years. The mean age of men in this registry was 61.0 (12.5) years (P<.001). On comparison of the 2 registries, both men and women in the GEMI database were slightly younger (P<.01). Most of the men were aged 55-64 years, but most women were older than 75 years. The distribution of cases was similar in both databases (Fig. 1). The proportion of patients admitted to public hospitals was similar (75.7% in the national database and 79.3% in the GEMI registry).
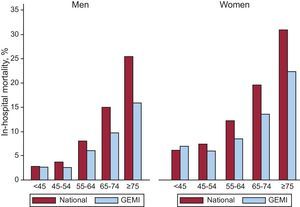
In-hospital mortality at a national level was 14.2%, and significantly higher among women than among men (20.4% vs 11.3%; P<.001). In the GEMI registry, in-hospital mortality was lower (9.2%), and was also greater among women (14.2% vs 7.3%; P<.001).
Analysis of the mortality trend by age group showed that it increased significantly with age in men and in women and in both registries analyzed. At a national level, in-hospital mortality among women ranged from 6.2% in those under 45 years to 30.9% in those aged ≥75 years; among men of the same groups, it ranged from 2.8% to 25.4% (P<.0001 for the trend). In-hospital mortality among women was significantly greater than that of men for all age groups in both databases (P<.01) (Fig. 2). There was no interaction between sex and age (P=.30) but it was significant between sex and Killip class (I-II vs III-IV; P=.001).
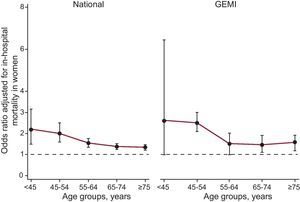
On evaluating the estimated risk of death (OR), young women were at greatest risk compared to men of the same age group. As age increased, this difference decreased, but the risk was always significantly higher in women. These findings were similar in both databases analyzed, although the variation between age groups was lower in the national registry; the risk decreased from OR=2.3 (1.5-3.3) in those under 45 years to OR=1.3 (1.2-2.4) in those aged 75 years or older, whereas the decrease was from OR=2.7 (1.1-6.8) to OR=1.5 (1.2-1.9) in the GEMI registry. After adjusting for socioeconomic level, the same trend persisted (Fig. 3). Although mortality was higher in the national registry than in the GEMI registry, given that the study aimed to assess the estimated relative risks and that the OR confidence intervals derived from the national database encompassed the point estimates of the OR derived from the GEMI registry, we proposed to using information from the GEMI registry to explore possible explanations for the difference in risk between men and women in the different age groups in large hospitals.
Estimated risk of in-hospital death due to myocardial infarction in women (compared to men) by age group, for the entire country and in the GEMI registry, 2001-2007. Odds ratio are adjusted for socioeconomic level. Men are taken as reference. GEMI, acute myocardial infarction multicenter study group.
No significant differences were observed between men and women in the time between symptoms onset and seeking medical attention.
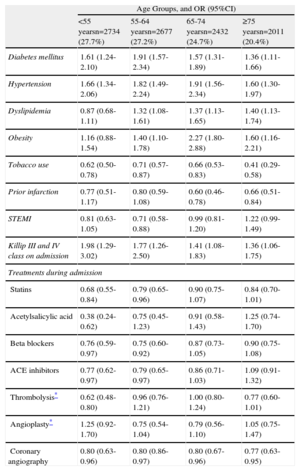
Table 1 shows the estimated risks in women for clinical characteristics, reperfusion procedures, and in-hospital treatment according to age. In all age groups, diabetes mellitus and hypertension were reported more frequently among women. Dyslipidemia and obesity were also more frequent among women, except in the youngest age groups. Tobacco use was higher among men in all age groups, as was prior infarction, although this difference was only significant above 65 years. With regard to the clinical condition on admission, in all age groups women were more likely to suffer severe heart failure (Killip class III-IV), and this difference was greater in the youngest groups (OR=1.98; 95%CI, 1.29-3.02). With regard to in-hospital pharmacological treatment, younger women had a lower probability of receiving treatments of proven clinical efficacy (statins, OR=0.68; 95%CI, 0.55-0.84; acetylsalicylic acid, OR=0.38; 95%CI, 0.24-0.62; and oral beta blockers, OR=0.76; 95%CI, 0.59-0.97). Likewise, the use of thrombolysis was lower (OR=0.62; 95%CI, 0.48-0.80). This difference remained when patients who were admitted with Killip class IV (OR=0.63; 95%CI, 0.48-0.81) were excluded from the analysis. In addition, in all age groups fewer coronary angiograms were undertaken in women.
Estimated Risks by Clinical Characteristics and In-hospital Treatment in Women Compared to Men for Each Age Group: GEMI Registry, 2001-2007.
| Age Groups, and OR (95%CI) | ||||
| <55 yearsn=2734 (27.7%) | 55-64 yearsn=2677 (27.2%) | 65-74 yearsn=2432 (24.7%) | ≥75 yearsn=2011 (20.4%) | |
| Diabetes mellitus | 1.61 (1.24-2.10) | 1.91 (1.57-2.34) | 1.57 (1.31-1.89) | 1.36 (1.11-1.66) |
| Hypertension | 1.66 (1.34-2.06) | 1.82 (1.49-2.24) | 1.91 (1.56-2.34) | 1.60 (1.30-1.97) |
| Dyslipidemia | 0.87 (0.68-1.11) | 1.32 (1.08-1.61) | 1.37 (1.13-1.65) | 1.40 (1.13-1.74) |
| Obesity | 1.16 (0.88-1.54) | 1.40 (1.10-1.78) | 2.27 (1.80-2.88) | 1.60 (1.16-2.21) |
| Tobacco use | 0.62 (0.50-0.78) | 0.71 (0.57-0.87) | 0.66 (0.53-0.83) | 0.41 (0.29-0.58) |
| Prior infarction | 0.77 (0.51-1.17) | 0.80 (0.59-1.08) | 0.60 (0.46-0.78) | 0.66 (0.51-0.84) |
| STEMI | 0.81 (0.63-1.05) | 0.71 (0.58-0.88) | 0.99 (0.81-1.20) | 1.22 (0.99-1.49) |
| Killip III and IV class on admission | 1.98 (1.29-3.02) | 1.77 (1.26-2.50) | 1.41 (1.08-1.83) | 1.36 (1.06-1.75) |
| Treatments during admission | ||||
| Statins | 0.68 (0.55-0.84) | 0.79 (0.65-0.96) | 0.90 (0.75-1.07) | 0.84 (0.70-1.01) |
| Acetylsalicylic acid | 0.38 (0.24-0.62) | 0.75 (0.45-1.23) | 0.91 (0.58-1.43) | 1.25 (0.74-1.70) |
| Beta blockers | 0.76 (0.59-0.97) | 0.75 (0.60-0.92) | 0.87 (0.73-1.05) | 0.90 (0.75-1.08) |
| ACE inhibitors | 0.77 (0.62-0.97) | 0.79 (0.65-0.97) | 0.86 (0.71-1.03) | 1.09 (0.91-1.32) |
| Thrombolysis* | 0.62 (0.48-0.80) | 0.96 (0.76-1.21) | 1.00 (0.80-1.24) | 0.77 (0.60-1.01) |
| Angioplasty* | 1.25 (0.92-1.70) | 0.75 (0.54-1.04) | 0.79 (0.56-1.10) | 1.05 (0.75-1.47) |
| Coronary angiography | 0.80 (0.63-0.96) | 0.80 (0.86-0.97) | 0.80 (0.67-0.96) | 0.77 (0.63-0.95) |
95%CI, 95% confidence interval; ACE, angiotensin-converting enzyme; OR, odds ratio; STEMI, ST-segment elevation myocardial infarction.
After adjusting for clinical characteristics, reperfusion procedures, and pharmacological treatment in the multivariate analysis, the risk of death persisted in the oldest and youngest groups (age<55 years and≥75 years), but only in women with ST-segment elevation myocardial infarction (STEMI). The effect was larger in the younger women (Table 2). After stratifying for Killip classes I-II vs III-IV and considering the interaction, the greater risk of death was only found in women aged <55 years with STEMI and in Killip class I-II (OR=4.27; 95%CI, 2.10-8.87), while a trend was observed in the group aged≥75 years (OR=1.50; 95%CI, 0.97-2.33).
Probability of In-hospital Death in Women Compared to Men With Adjustment for Age and Type of Infarction. GEMI Registry, 2001-2007.
| Age | STEMI nn=6151 (72.7%) | NSTEMIn=2312 (27.3%) |
| ORa (95%CI) | ORb (95%CI) | |
| <55 years | 2.49 (1.29-4.82) | 0.54 (0.09-3.36) |
| 55-64 years | 1.11 (0.67-1.86) | 0.96 (0.41-2.24) |
| 65-74 years | 1.42 (0.96-2.10) | 0.94 (0.43-2.02) |
| ≥75 years | 1.49 (1.05-2.11) | 1.26 (0.72-2.20) |
95%CI, 95% confidence interval; NSTEMI, non-ST-segment elevation myocardial infarction; OR, odds ratio; STEMI, ST-segment elevation myocardial infarction.
Adjusted for history of diabetes mellitus, hypertension, prior infarction, Killip class on admission (I-II vs III-IV), in-hospital treatments (acetylsalicylic acid, statins, angiotensin-converting enzyme inhibitors, oral beta blockers), thrombolysis, and angioplasty (these models were able to correctly classify by age:<55 years, 97%; 55-64 years, 95%; 65-74 years, 91%; and≥75 years, to 84%).
Adjusted for history of diabetes mellitus, hypertension, prior infarction, Killip class on admission (I-II vs III-IV), and in-hospital treatments (acetylsalicylic acid, statins, angiotensin-converting enzyme ACE inhibitors, oral beta blockers) (these models were able to correctly classify by age:<55 years, 98%; 55-64 years, 95%; 65-74 years, 94%; and≥75 years, 89%).
The sensitivity analysis did not show statistically significant differences in the estimated risk of any of the age groups (results not shown).
DiscussionThe present study confirms the greater risk of in-hospital death due to AMI in women compared to men. In addition, it provides evidence of the heterogeneous prognosis in women who are hospitalized for AMI, as younger women have a higher risk of in-hospital death than men of the same age. Similar results have been reported in other studies, which have identified women younger than 55 years as the group at highest risk after adjusting for confounding factors.20 Our results support this relationship in a different context, ie, a Latin American country. Although AMI is not common in young women, its impact on the family, social, and work environment make it an important problem.
Some explanations for these findings point to contextual factors, such as the lower level of income usually seen in women, or have a direct relationship with the clinical characteristics and medical care received. In this study, the effect of female sex as a risk factor for death was not affected by adjusting for socioeconomic level (type of hospital). The time elapsed between onset of symptoms and diagnosis did not show any differences by sex. In principle, a sex-based difference could have been a possible explanation for the greater mortality in women, as it has an impact on the possibility of receiving reperfusion therapy, which reduces both acute and long-term mortality.21–24 With regard to the differences in the presentation of AMI, young women did not have a higher prevalence of risk factors other than older age, but women under 55 years had a greater incidence of severe heart failure at the time of admission. The prognostic value of Killip functional class has been documented in large studies. It has been shown that patients with more severe Killip classes have a lower chance of receiving pharmacological treatment and percutaneous revascularization procedures, and the risk of death in the acute phase of infarction is 2-fold higher.25,26
With regard to in-hospital management, a lower use of coronary angiography was observed in women, regardless of age, thereby limiting the possibility of undergoing myocardial revascularization procedures. Vaccarino et al13 have reported this trend in an analysis of more than half a million patients with AMI; coronary angiography was used less in women than in men, even after adjusting for multiple factors. In addition, in the present study, women younger than 55 years received fewer thrombolytic agents (eligible patients), statins, acetylsalicylic acid, and beta blockers during hospitalization. Other studies, both international and conducted in Chile, had already reported this gap in treatment, but without reference to age group.3,6,13
In addition, the characteristics of extrahospital mortality due to AMI could in part explain the results obtained. There is evidence that the majority of men die in the early phase and do not arrive at hospital; thus, those who do manage to get to a hospital have the best prognosis. International studies and a study conducted in Chile between 1997 and 2007 have shown that men have a higher risk of dying before reaching hospital,27–29 possibly associated with a higher incidence of high mortality events in the first hours of infarction.
The greater risk of death due to AMI in women younger than 55 years was maintained after adjusting for clinical characteristics and treatment characteristics, but only among women in Killip class I and II on admission and not for those who were admitted with Killip class III and IV. With regard to the prognosis for patients in shock, Wong et al.,30 using data from the SHOCK Trial Registry, did not find any significant differences in mortality due to sex, even after adjusting for clinical and treatment variables.
Differences in some pathophysiological characteristics could explain the greater risk observed in younger women. It has been reported that they have less developed collateral vessels, along with a higher incidence of vasospasm, hypercoagulable states, and endothelial and smooth muscle dysfunction. In addition, in this group, it has been observed that the infarction mechanism is more often due to erosion than to rupture of an atherosclerotic plaque.31–34
Strengths and Limitations of the StudyThe biggest strength of this study is that it included all cases of AMI in Chile during the study period, thereby ensuring that the findings of the in-hospital mortality analysis by age and sex were reliable. The GEMI registry was used to search for possible factors that might explain the greater mortality observed among women; however, given the characteristics of the registry and because it was a non-probabilistic sample, it was not possible to make firm inferences of the results for the entire population. This is one of the limitations of the study. In addition, this was a sample of the GEMI registry. Thus, only data from large hospitals were used (those with coronary units and many of them with catheterization laboratories) and mortality was lower. In addition, patients of lower clinical risk with satisfactory progress in smaller hospitals would not be sufficiently represented. This may generate a selection bias that overestimates the higher risk of death among women in this sample. However, in normal clinical practice, most patients are admitted to large hospitals or, after receiving acute therapy, are transferred to smaller hospitals to complete treatment and subsequent coronary angiography.
Another limitation is the lack of continuity in the participation of the hospitals during the study period. This could also introduce a selection bias, even though more than 80% of the sample was obtained from hospitals that contributed to the registry for the 7 years analyzed.
ConclusionsYoung women with AMI have a higher in-hospital mortality than men, particularly in the group younger than 55 years. The excess risk is maintained after adjustment for socioeconomic level, clinical characteristics, and treatment differences, but only in the group of patients with STEMI and in Killip class I-II. This suggests that other variables could be implicated in this phenomenon. A more aggressive diagnostic and therapeutic approach is required in this group of women. This is even more so given the important role of young women in the family and society. These results observed in Chile could be representative of the situation in other Latin American countries with a similar level of development. This would help with the sharing of experience with successful interventions to control AMI in women.
Conflicts of interestNone declared.
To the researchers and collaborators of GEMI Registry of the participating hospitals.