This article summarizes the main developments reported during the year 2012 concerning ischemic heart disease, together with the most relevant innovations in the management of acute cardiac patients.
Keywords
.
EPIDEMIOLOGY, PATHOGENESIS, AND SECONDARY PREVENTIONAlthough total cardiovascular disease mortality decreased 30% between 1998 and 2008,1 coronary artery disease remains a major cause of morbidity and mortality in industrialized countries. In fact, ischemic heart disease is the leading cause of cardiovascular death and accounts for between 30% and 50% of all deaths.2,3 In Spain, ischemic heart disease causes nearly one-tenth of all deaths, rising to one-sixth in the United States.3
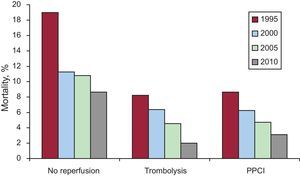
Recently, data from several national French registries have been updated, showing a 68% reduction (from 13% to 4%) in early (30-day) mortality in patients with ST-segment elevation acute myocardial infarction (STEMI) during the last 15 years.4 This reduction in mortality is explained not only by better health care, but also by the epidemiological changes occurring in the population, as shown by improvements even in patients not undergoing reperfusion (Fig. 1). In Spain, data from the PRIAMHO I, PRIAMHO II, and MASCARA registries demonstrate that between 1995 and 2005 there was also a significant reduction in early mortality in patients with STEMI, from 12.6% to 6%.5
Trends in mortality from ST-segment elevation acute myocardial infarction according to type of reperfusion therapy administered. PPCI, primary percutaneous coronary intervention. Adapted from Palacios et al.5 with permission.
Despite these encouraging data, much remains to be done. For example, a Spanish registry of over 11 000 patients analyzed long-term prognosis after infarction. A high rate of readmissions was found, which the authors correlated with coexisting cardiovascular risk factors6–8 whose control is frequently suboptimal. These facts highlight the need to improve secondary prevention strategies.
Genetics and Cardiovascular Risk FactorsKnowledge of the human genome has provided more information on the contribution of genetic factors to the emergence and development of ischemic heart disease. A study based on blood samples obtained in the WOSCOPS registry found an association between the Y chromosome and the risk of coronary artery disease in European men, through genes involved in inflammation and the immune response.1 In the same line, another study, which analyzed 25 000 patients enrolled in 12 studies, found associations between various polymorphisms and coronary events, involving risk factors other than the classically established ones.9 The association between the expression of 8 specific loci in the human genome and the activity and concentration of lipoprotein phospholipase A2, which is related to the development of coronary artery disease, has been demonstrated in a meta-analysis of 13 664 patients.10
With respect to cardiovascular risk factors, several American population studies have demonstrated reductions in the prevalence of smoking, hypertension, and hypercholesterolemia, increases in obesity and diabetes mellitus, and no change in physical activity levels.3,11 In an American registry of 50149 patients with acute myocardial infarction, extreme obesity (body mass index>40) was associated with higher in-hospital mortality despite presenting a favorable coronary anatomy and ventricular function and undergoing similar treatment patterns.12 In a meta-analysis of nearly 4 million individuals, smoking in men was associated with a 25% increase in the risk of coronary heart disease compared to women; however, the interference of other environmental factors could not be ruled out.13
DIAGNOSTIC TECHNIQUESIn patients with suspected acute coronary syndrome (ACS), coronary artery calcium scores on computed tomography (CT) add predictive information, whereas other variables (such as C-reactive protein and natriuretic peptide) provide no additional information.14 The role of coronary CT angiography in the emergency department for patients with suspected ACS was evaluated in the ROMICAT II study.15 The study included 1000 patients with chest pain, normal electrocardiogram (ECG) findings and negative troponin test. Patients were assigned to CT angiography or standard evaluation (serial troponins). The primary endpoint was duration of hospital stay. The mean time to diagnosis was 10.4 h in the CT angiography group and 18.7h in the control group (P=.001); hospital stay among patients in the CT angiography group was reduced by an average of 7.6 h (P=.002) and more patients from this group were discharged directly from the emergency department (47% vs 12%; P<.001). The ACS ratio was 8%, with no undetected ACS in the 2 groups and no significant differences between the groups in events at 28 days. The patients in the CT angiography group received greater radiation exposure, but the cumulative cost of both strategies was similar. Another clinical trial also has supported the safe discharge of intermediate-risk patients with suspected ACS from the emergency department, based on information from CT angiography.16 However, these studies were conducted in highly selected centers with optimal conditions (widely available CT angiography and proven expertise) and thus it may be difficult to extrapolate their results. In addition, the potential side effects of the technique (excess radiation exposure, use of contrast medium) and the absence of real clinical benefit argue the need for great caution in generalizing the results to patients with chest pain and no clinical risk factors.17
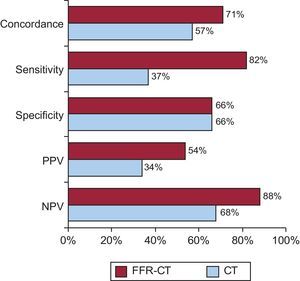
The noninvasive determination of fractional flow reserve by CT angiography appears to have greater diagnostic accuracy than CT angiography alone for the study of stable coronary artery disease18 (Fig. 2).
Concordance, sensitivity, specificity, positive predictive values, and negative predictive values of fractional flow reserve calculated from computed tomography (cutoff, 0.80) and computed tomography stenosis>50% calculated from computed tomography compared to functional significance obtained by the invasive estimation of fractional flow reserve (cutoff, 0.80). Adapted from Min et al.18 with permission. CT: computed tomography; FFR-CT, fractional flow reserve calculated from computed tomography; NPV, negative predictive values; PPV, positive predictive values.
A recent study has shown that measuring growth differentiation factor 15 (GDF-15) levels on admission improves the predictive value of the GRACE score, a validated scoring system that is recommended in the guidelines. In a study including 1122 patients with non-ST-segment elevation acute coronary syndrome (NSTEACS), the use of this marker reclassified 31% of patients without events as low risk and 27% of patients with events as high risk.19 Similarly, measuring N-terminal pro-B-type natriuretic peptide levels enhances the predictive value of the GRACE score.
The role of high-sensitivity troponin T in identifying NSTEACS in individuals with normal conventional troponin was the focus of a study that included 446 patients with chest pain seen in the emergency department. Although elevated high-sensitivity troponin T levels reclassified 19% of the patients into the NSTEACS category, their additive prognostic value to classic clinical and electrocardiographic variables was marginal. However, it was found that levels≤3 ng/L provided high negative predictive value.20
An interesting translational study has shown that metabolic profiling can be very useful in the early management of patients with acute myocardial ischemia.21
SPECIAL ASPECTS OF ISCHEMIC HEART DISEASE IN ELDERLY INDIVIDUALS AND WOMENMedical Treatment and Reperfusion Therapy in OctogenariansIn elderly patients, medication use and revascularization are still under-prescribed compared to what is recommended in the guidelines. In a study which included 213 patients with ischemic heart disease aged≥80 years, angiotensin-converting enzyme inhibitors, beta blockers, statins, and acetylsalicylic acid were prescribed to 43%, 56%, 56%, and 66% of patients, respectively, without the degree of comorbidity influencing medication use.22 A registry that included patients admitted with NSTEACS aged≥85 years suggested that an interventional approach was associated with increased survival and fewer ischemic events than conservative management, and that the benefits were maintained after minimizing selection bias using a propensity score.23 The reperfusion rate in a large sample of elderly individuals≥80 years admitted with STEMI in the United States in the period 2004-2008 was<50%, although the proportion of patients undergoing mechanical revascularization has increased in the last decade.24 A similar Spanish single-center study conducted between 2005 and 2011, which included 102 elderly patients aged≥85 years, demonstrated a reperfusion rate of 68%, although the proportion undergoing fibrinolysis was greater.25
Coronary Artery Bypass Grafting in Elderly PatientsAlthough greater long-term survival has been reported among patients aged>65 years with multivessel disease who had undergone coronary artery bypass grafting (CABG) versus percutaneous coronary intervention (PCI),26 in a sample of 476 octogenarians with 3-vessel disease complete revascularization was not significantly better than incomplete revascularization.27 Two randomized trials have demonstrated similar mortality rates (at 30 days and at 6 months) after CABG with or without cardiopulmonary bypass.28,29 A subanalysis of the CUSTOMIZE registry showed that CABG was superior to PCI with drug-eluting stents in younger patients with unprotected left main coronary artery disease; however, this advantage disappeared in patients aged≥75 years.30
Sex-based Differences: The Case of WomenRecent studies31,32 have concluded that, compared to men, young women with ACS have higher mortality rates. However, this difference disappears with age and long-term prognosis among the elderly is actually better for women. In stable coronary artery disease, sex does not appear to be an independent prognostic factor33; however, in both acute and chronic coronary artery disease, fewer women undergo revascularization than men, although absence of epicardial coronary disease is more common among women.31–33
NON-ST-SEGMENT ELEVATION ACUTE CORONARY SYNDROMEAntithrombotic TherapyThe results of the TRACER study were published this year. The study included 12944 patients with NSTEACS treated with acetylsalicylic acid and clopidogrel who were randomized to receive vorapaxar or placebo.34 Vorapaxar is an oral protease-activated-receptor 1 antagonist which inhibits thrombin-induced platelet activation; in the preclinical study, it showed a good safety profile. The primary endpoint of the TRACER study was the incidence of cardiovascular death, myocardial infarction, stroke, recurrent ischemia, or urgent coronary revascularization at 2 years. This endpoint occurred in 18.5% of patients treated with vorapaxar and 19.9% of those treated with placebo (P=.07). Moderate or severe bleeding (7.2% vs 5.2%; P<.001) and intracranial hemorrhage (1.1% vs 0.2%; P<.001) were more common in the vorapaxar group. To summarize, in patients with NSTEACS the addition of a third oral antiplatelet agent, vorapaxar, to standard therapy provided no added benefit.
The TRILOGY ACS study investigated the efficacy of prolonged treatment with prasugrel versus clopidogrel in 7243 patients with NSTEACS receiving conservative treatment (without coronary angiography or planned revascularization).35 The primary endpoint was the incidence of cardiovascular death, myocardial infarction or stroke at a mean follow-up of 17 months. The endpoint occurred in 13.9% of patients treated with prasugrel and in 16% of those treated with clopidogrel (P=.21). The prasugrel dose (5 mg daily) was adjusted for patients aged>75 years and for those weighing<60 kg. The incidence of major and intracranial bleeding was similar in both groups, although mild and moderate bleeding were more frequent with prasugrel. The authors concluded that the long-term use of prasugrel in patients with NSTEACS treated conservatively was not superior to clopidogrel for reducing the primary endpoint, although the risk of major bleeding remained low.
The ISAR-REACT 4 study included 1721 patients with high-risk NSTEACS undergoing PCI who were randomized to receive bivalirudin or abciximab plus heparin before PCI,36 after receiving treatment with acetylsalicylic acid (250 mg to 500 mg) and clopidogrel (600-mg loading dose). The primary endpoint was the 30-day incidence of death, infarction, new revascularization or major bleeding. The endpoint occurred in 10.9% of the patients treated with abciximab plus heparin and in 11.0% of those treated with bivalirudin (P=.94). A secondary endpoint was major bleeding at 30 days, which was lower in the bivalirudin group (2.6% vs 4.6%; P=.02). These results were consistent and confirmed the safety of bivalirudin in patients with NSTEACS undergoing PCI, in the same way that the HORIZONS-AMI study demonstrated its safety in patients with ST-segment elevation acute coronary syndrome (STEACS) undergoing primary PCI (PPCI). On the other hand, it should be noted that the ISAR-REACT 4 study did not include high-risk patients and that the results are difficult to extrapolate to patients treated via radial access or with new antiplatelet agents.
The ATLAS ACS 2-TIMI 51 was a major study published this year.37 The study assessed rivaroxaban, an oral factor Xa inhibitor, at doses of 2.5 mg or 5 mg every 12h, initiated in the week following the ACS. A total of 15 526 patients were randomized to receive rivaroxab or placebo with a mean follow-up of 13 months (maximum follow-up, 31 months), during which period the primary endpoint was the incidence of cardiovascular death, myocardial infarction, or stroke. This endpoint occurred in 8.9% of the patients treated with rivaroxaban versus 10.7% in those treated with placebo (hazard ratio=0.84; P=.008). The 2.5-mg dose of rivaroxaban also reduced cardiovascular mortality during follow-up (2.7% vs 4.1%; P=.002). On the other hand, the patients treated with rivaroxaban had increased rates of major bleeding (2.1% vs 0.6%; P<.001) and intracranial hemorrhage (0.6% vs 0.2%; P=.009), but without a significant increase in fatal bleeding (0.3% vs 0.2%; P=.66). This study marks a new stage in anticoagulant therapy as secondary prevention in ischemic heart disease, especially for patients with a low risk of bleeding.
Revascularization StrategyA recent meta-analysis supported the guidelines that recommend an invasive strategy for diabetic patients with NSTEACS.38 Nine trials that compared an invasive and a conservative strategy were analyzed. They included 9904 patients with NSTEACS, of whom 1789 (18.1%) had diabetes mellitus. At 12 months, the absolute risk reduction in nonfatal myocardial infarction with an invasive strategy was greater in diabetic patients than in nondiabetic patients (3.7% vs 0.1%; P interaction=0.02), with no difference in mortality or stroke between the 2 groups (P interactions 0.68 and 0.20, respectively).
On the other hand, the 5-year prognostic impact of revascularization procedure-related myocardial infarction in patients with NSTEACS was recently investigated using the FRISC II, ICTUS, and RITA-3 data set.39 Long-term mortality rate was similar in patients who experienced procedure-related myocardial infarction and those who did not, whereas the rate was significantly higher in patients who had a spontaneous infarction within 6 months after revascularization.
ST-SEGMENT ELEVATION ACUTE MYOCARDIAL INFARCTIONMechanisms and Prognostic StratificationThe analysis of coronary thrombi underlying STEMI, based on material aspirated during PPCI, has provided information on some of the characteristics associated with an increased risk of distal embolization and impaired reperfusion. A study that included 178 patients showed that erythrocyte-rich thrombi lead to impaired myocardial reperfusion and late remodeling.40 The presence of thrombus is not always evident on angiography, especially in women. A study that included 51 women with STEMI without significant angiographic lesions detected plaque disruption on intravascular ultrasound in 38% of the patients and signs of necrosis on cardiac magnetic resonance imaging in 59%41; this indicates the possible involvement of embolization or vasospasm in the pathogenesis of STEMI in women without severe coronary lesions.
New cell groups that are relevant in the acute and subacute phases of STEMI continue to be studied. In the acute phase, a significant increase in the number of endothelial progenitor cells has been observed. In a group of 32 patients this increase was particularly common in patients with single-vessel disease.42 Although monocytes/macrophages play a key role in myocardial healing, an experimental study has demonstrated that regulatory CD4+ T-cells are also important and that their absence or inhibition hinders this process.43
An ECG is a fundamental tool in the diagnosis and management of STEMI. Classic, easily detectable signs indicate an unfavorable prognosis. Thus, right bundle branch block was detected in 6% of cases in a registry that included 6742 patients. Both in-hospital mortality (14%) and cardiogenic shock (16%) were identical in patients with left bundle branch block.44 The prognostic impact was concentrated in patients with new onset right bundle branch block, which had the highest mortality rate (19%) compared to patients with new left bundle branch block (13%), old left bundle branch block (10%), and old right bundle branch block (6%). The presence of acute ST-segment elevation in lead aVR increases the risk of death, which at 1 month was >22% for both anterior and lower infarction.45
TreatmentA randomized study compared 300-mg and 600-mg clopidogrel loading doses in 201 patients undergoing PPCI for STEMI. Pretreatment with 600mg was associated with smaller infarct size, better angiographic results, better preservation of systolic function, and fewer events at 30 days.46
A randomized study of 452 patients with anterior STEMI analyzed the effect of manual aspiration thrombectomy and intracoronary abciximab in reducing infarct size in patients undergoing PPCI with bivalirudin anticoagulation. As assessed by cardiac magnetic resonance imaging, intracoronary abciximab, but not aspiration thrombectomy, reduced infarct size at 30 days.47 Drug-eluting stents continue to be a good choice in the invasive treatment of STEMI compared to bare-metal stents and to drug-eluting balloons plus bare-metal stents.48
Cardiac magnetic resonance imaging has become a technique of choice for assessing myocardium salvaged by various reperfusion strategies in patients with STEMI (Fig. 3). In a group of 118 patients it was observed that the determining factor in salvaging a significant amount of myocardium (>30%) was delay to revascularization, rather than the type of strategy, whether PPCI or pharmacoinvasive.49 The Achilles heel of a pharmacoinvasive strategy is the need for rescue angioplasty: in a series of 50 patients treated with rescue angioplasty, only 3% of the myocardium was salvaged.50
Cardiac magnetic resonance imaging provides excellent quantification of the myocardium salvaged by reperfusion, due to the possibility of comparing the areas of risk and the areas of necrosis. A and B: Areas of hyperintensity representative of the area at risk (upper) and the area of necrosis (late gadolinium enhancement images, lower) in short-axis view; patient A was reperfused 340 min after the onset of pain and had a myocardial salvage index of 16; patient B was reperfused 115 min after the onset of pain and had a myocardial salvage index of 82%. Reproduced from Monmeneu et al.49 with permission.
There is continuing effort to limit reperfusion injury. In a randomized trial that included 871 patients, out-of-hospital treatment with glucose-insulin-potassium versus placebo did not reduce infarct progression or short-term events.51 Data on ischemic postconditioning after PPCI are contradictory; whereas a randomized study of 79 patients found no reduction in infarct size and even a trend toward greater injury,52 a different series that included 50 patients found less edema and infarction in the treated group.53 Thus, more clinical and experimental information is needed to develop new therapies to add to the great advances achieved in the prognosis of STEMI during recent decades.
CARDIAC CRITICAL CAREThis year has seen the publication of important studies in the field of cardiopulmonary resuscitation. The ROC PRIMED study was a cluster randomized trial that included 9933 adult patients with out-of-hospital cardiac arrest (OHCA). The study compared a strategy in which patients received 30s to 60s of cardiopulmonary resuscitation before early analysis of cardiac rhythm to one in which the patients received 3min of resuscitation before the analysis of cardiac rhythm with subsequent defibrillation when indicated.54 The percentage of patients discharged without significant functional limitations—the primary endpoint—was 5.9% in both arms. The results show that neither of the resuscitation strategies was superior to the other, although it should be emphasized that adherence to the stipulated times was not perfect and that due to ethical considerations cardiac massage was administered to all patients before assessing cardiac rhythm.
The administration of epinephrine has been one of the mainstays of cardiopulmonary resuscitation for decades, despite a lack of evidence that this drug improves patient prognosis and results of observational studies and clinical trials suggesting that it may have a detrimental effect, especially at high doses. The results of the largest study ever conducted on the effects of epinephrine administered before hospital arrival in patients with OHCA were published this year. The study included 417 188 patients and demonstrated that whereas the use of epinephrine was associated with an increased probability of return of spontaneous circulation (18.5% vs 5.7%), there was a significantly decreased probability of survival (5.4% vs 4.7%) and good functional recovery at 1 month.55 Although these results were confirmed in subgroups defined by similar propensity scores, they cannot be considered definitive, given that the study was observational. Nevertheless, the results provide support for a placebo-controlled clinical trial that would unambiguously clarify the role of epinephrine in the resuscitation of patients with OHCA.
Another study retrospectively analyzed the association between chest compression rate during the first 5 min of resuscitation and survival to hospital discharge in 3098 patients with OHCA.56 The results confirmed previous observations that a rapid compression rate is more effective to return spontaneous circulation (120 bpm being the optimal rate), although the compression rate was not associated with survival. It has been reported that the immediate benefits of revascularization and therapeutic hypothermia for postresuscitation treatment in patients with OHCA persist at 5-year follow-up.57
Few efforts in the field of cardiac critical care have aroused more interest than 2 recent clinical trials that questioned the benefits of intra-aortic balloon counterpulsation (IABC). The AMI CRISP study included 337 patients with anterior STEMI but without cardiogenic shock treated with PPCI. Circulatory support through an intra-aortic balloon pump (IABP) placed prior to PPCI and maintained for at least 12 h did not reduce infarct size as measured by cardiac MRI performed 3 days to 5 days after PPCI.58
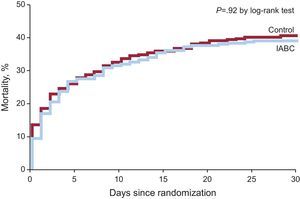
The results of the IABP-SHOCK II study59 were even more striking. The study randomized 600 patients with cardiogenic shock complicating NSTEMI of>12 h duration to IABP support or no IABP support. NSTEMI was not due to mechanical complications and most of the patients were treated with PCI. The IABP was placed before or immediately after PCI and was maintained until hemodynamic stabilization was achieved. The primary endpoint of 30-day mortality occurred in 39.7% of patients in the IABP group and 41.3% in the control group (no significant differences). The results did not change significantly after adjusting for several prognostic variables and were very similar in the different subgroups (Fig. 4). Although IABC offered some protection against multiorgan dysfunction, the effect was transient and was not associated with significant benefits in time to hemodynamic stabilization, need for vasoactive medication, serum lactate levels, or renal function. Before generalizing these results, some special aspects of the study should be taken into account, such as the high proportion of patients who required resuscitation before randomization (45%), those who received therapeutic hypothermia (38%) (indicating that a large proportion had experienced an OHCA), or the relatively low proportion of patients with anterior STEMI (42%) or tachycardia (only 25% had a heart rate>110 bpm). Given these considerations, and pending further analysis to help better interpret these results and identify subgroups that would benefit most from IABC, this study appears to challenge the level of recommendation of this therapy in the clinical practice guidelines and the frequency of its use in patients with AMI and cardiogenic shock.
Kaplan-Meier curves for all-cause mortality during the first 30 days after randomization in patients enrolled in the IABP-SHOCK II study. IABC, intra-aortic balloon counterpulsation. Reproduced with permission from Thiele et al.59 with permission.
Other studies have drawn attention to the adverse long-term prognostic significance of heart failure during admission60 and of nosocomial anemia in the absence of bleeding in patients with ACS.61
CONFLICTS OF INTERESTNone declared.