To the Editor,
Heart resynchronization therapy (HRT) is accepted in selected patients with heart failure. A persistent problem with the electrode implanted in the coronary sinus (CS) for left ventricular stimulation is that it can migrate either early or late. This involves possible loss or worsening of function and/or the possibility of phrenic stimulation, with consequent more or less frequent diaphragm contractions that are very unpleasant for the patient.1 Sometimes the problem can be resolved by means of device reprogramming, but not in others cases. Recently there has been a report of re-placement of this electrode pulling it with a steerable catheter introduced into the femoral vein, in 9 patients, with phrenic stimulation by early distal electrode displacement. Once it is repositioned, the authors place a stent in place compressing the electrode against the vein wall to achieve definitive stabilisation. Time from implant was 6 (6) months, with stability and good function after a follow-up of 7.7 (4.6) months.
We present the case of a 65-year-old patient with severe left ventricular dysfunction, advanced left His bundle block, without coronary atherosclerosis, with a cardiogenic profile syncope, and implanted 43 months ago with an automatic HRT defibrillator. The implant was satisfactory in a posterolateral CS vein, with a stimulation threshold in the left ventricle of 2.1 V at 0.5 ms, with no phrenic stimulation at 10 V. Six months after implant placement the patient began to suffer occasional phrenic stimulation and on x-ray it was possible to see a slight distal displacement of the CS electrode, at that moment the problem was corrected by reprogramming. However, 10 months later phrenic stimulation reappeared. Initially the patient was in acceptable conditions, since the excellent stimulation threshold was at levels that did not cause said stimulation or this was only occasional or postural. After 3 years of implant placement the problem became continuous and disabling, and could not be fixed by reprogramming. It was decided to replace the generator (which is practically in ERI) and replace or change the electrode. The patient had an excellent cardiological condition since implant, and there was no doubt as to the need for the HRT.
Before the replacement, and in agreement with the patient, percutaneous re-placement was attempted, following the experience mentioned above, in spite of not having found in the literature cases with electrodes implanted for such a long time. In spite of the fact that CS electrodes are placed by passive fixation, there may be a fibrotic reaction of surrounding tissue related especially, to time of implant.2 The appearance of adhesions could make the procedure difficult or impossible, or could create complications.
A Mariner (Medtronic, Minneapolis, USA) ablation catheter was introduced through the right femoral vein up to the right atria through a DAIG (DAIG, St. Jude Medical, USA) SR0 long sheath that was directed to the CS after having introduced the distal portion of the ablation catheter in its distal portion as if it were a guide.
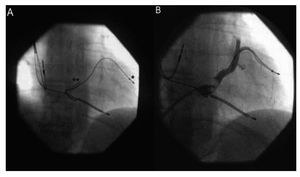
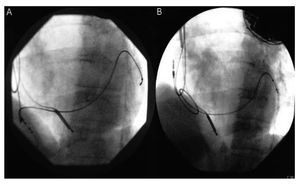
Once the catheter was withdrawn, an angiography was performed to reassess CS anatomy with the idea of carrying out a replacement (Figure 1). Subsequently, the system was withdrawn from the right atria and with the tip of the ablation catheter at its maximum curvature, the electrode was hooked, and it was pulled softly into the inferior vena cava (Figure 2). The electrode was moved without any difficulty, and phrenic stimulation immediately ceased. The final stimulation threshold was 2.4 V at 0.5 ms. Given the fact that the generator was soon to be replaced we did not place a holding stent, since this could cause difficulty in manipulating the electrode if the result turned out to be transient.
Figure 1. A: position of the electrode in the coronary sinus (CS)(*) in an oblique right position before collection, with a long sheath in the CS(**). B: CS angiography.
Figure 2. A: traction of the electrode. B: position of the electrode at the end of traction.
The procedure was carried out with echocardiographic monitoring and with previous warning of the heart surgery department that there could be need for emergency surgery. However, there were no complications.
This change was performed 2 months after re-placement, sufficient time to consider the position of the electrode as stable, with similar stimulation parameters and total absence of phrenic stimulation.
In conclusion, percutaneous traction of an electrode in the CS can be carried out even several years after implantation. In our opinion, given the ease of this procedure, it is worth attempting, so as to avoid a much more complicated and risky procedure.