Regular physical exercise is an established recommendation for preventing and treating the main modifiable cardiovascular risk factors, such as diabetes mellitus, hypertension, and dyslipidemia. Performing physical activity of moderate intensity for a minimum of 30min 5 days a week or of high intensity for a minimum of 20min 3 days a week improves functional capacity and is associated with reductions in the incidence of cardiovascular disease and mortality. Physical exercise induces physiological cardiovascular adaptations that improve physical performance, and only in extreme cases can these adaptations lead to an increased risk of physical exercise-associated complications. The incidence of sudden death or serious complications during physical exercise is very low and is concentrated in people with heart diseases or with pathological cardiac adaptation to exercise. Most of these cases can be detected by cardiology units or well-trained professionals.
Keywords
The human body, and particularly the cardiovascular system, is the result of an evolutionary process aimed at increasing resistance to the environment. Current understanding of the physiology of different species indicates that humans developed their systems evolutionarily, compared with reptiles, amphibians, and even other mammals, to become more resistant to a lack of food or water and prolonged physical activity.1 However, the progressive increase in life expectancy and certain lifestyle and dietary changes in the last 6 decades have exposed the human species to threats for which it is not prepared or biologically adapted. Most factors determining this new vital scenario are directly related to the development of risk factors and cardiovascular diseases,2 which have become the leading cause of death in the last century alone3; the predominance of cardiovascular disease has led to a search for treatments that, in some cases, modify even certain adaptive mechanisms that the human body has developed during the course of evolution.4 In contrast, regular physical exercise is an established recommendation for the treatment of the main modifiable cardiovascular risk factors, such as diabetes mellitus,5 hypertension,6 and dyslipidemia,7 as well as excess weight, although exercise is one of the least implemented measures by both physicians and patients.8
EPIDEMIOLOGYA sedentary lifestyle is defined as one that does not comply with the recommendations for the practice of physical activity of moderate intensity for a minimum of 30min 5 days a week or of high intensity for a minimum of 20min 3 days a week.9 In recent decades, the prevalence of sedentary individuals has slightly decreased; although somewhat contrasting data have been reported, between 20% and 40% of the population can be considered sedentary.10–13 Moreover, although knowledge of energy requirements is important for adjusting and individualizing nutritional recommendations, measurement of energy consumption is difficult in routine clinical practice; thus, objectives to combat sedentary lifestyles should aim to increase physical activity to achieve, or even exceed, the general recommendations.9
The majority of people devote a considerable portion of their day to work, which is usually used to justify a lack of physical exercise. Nonetheless, physical activity performed during work also confers protection against cardiovascular disease. Midway through the last century, physical activity performed during working hours was found to explain the difference in the incidence of cardiovascular complications among workers in a single company: bus drivers had more acute myocardial infarctions than conductors who climbed the stairs of double-decker London buses hundreds of times a day,14 a difference that was also seen between post office workers and mail carriers or delivery workers.15 Thus, physical activity performed during work confers substantial protection against cardiovascular diseases; however, physical activity during working hours has clearly been reduced by changes in recent decades.10,11 This development can be explained by the progressive automation and sophistication of factory production lines, which have decreased the physical effort expended by workers, who now merely monitor the machinery. From the point of view of cardiovascular prevention, this situation has become crucial, and workers not performing office work now show a more unfavorable cardiovascular risk profile than office workers. In an extensive registry of workers in Spain, manual workers showed more obesity, hypertension, and metabolic syndrome than office workers and managers.16
PROTECTIVE MECHANISMS OF SPORTPhysical exercise is defined as any body movements produced by the locomotor system to contract and relax muscles that involve energy consumption. This movement generally increases oxygen and nutrient use by the muscles. Muscle adaptation to exercise is the basis of exercise training, and is measured both by the adaptation and development of muscle fibers and by changes in their metabolism, chiefly in mitochondria.17 Muscle adaptation is a complex and poorly understood process that involves pathways as diverse as calcineurin receptors, neoangiogenesis, increased gene expression, mitochondrial metabolic reprogramming, and myosin synthesis from muscular tissue itself. However, the effect of muscle adaptation is not only vital in muscles, as it has been linked with delayed aging via stabilization of mitochondrial telomerase.18
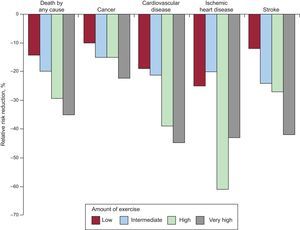
Functional capacity and the amount of exercise are inversely correlated with the development of cardiovascular risk factors19 and with long-term mortality from cardiovascular and neoplastic diseases (Figure 1).20 A striking example of this relationship was revealed in a comparative study of the long-term prognosis of an extensive sample of participants in the Tour de France vs the general population, which showed that the cyclists had a 41% lower rate of mortality, from both neoplasms (44%) and cardiovascular diseases (33%).21
Effect of physical exercise on the incidence of various diseases according to Wen et al.20
Cardiovascular adaptation with training mainly involves the following: a) an increase in stroke volume; b) an increase in heart cavity volume and wall thickness; c) a decrease in heart rate both at rest and during submaximal exercise, and d) an improvement in myocardial perfusion.22
Cardiac output increases during physical activity due to an increase in heart rate and stroke volume.23 During intense exercise, stroke volume can even be doubled; although this increase is barely noticeable in untrained people, it is considerable and continues until it reaches a maximum at levels of effort of between 50% and 60% of maximum oxygen consumption in fit athletes.23 At this level of effort, the stroke volume stabilizes until very high exercise intensities.
Another functional adaptation related to regular physical exercise involves an increase in both cardiac chamber volume and wall thickness; an increase in the former is the most important factor for increasing cardiac output.24 In athletes that perform aerobic endurance exercise, cardiac chamber volume predominates, although wall hypertrophy also develops after many years of high-intensity training.25 In contrast, very small changes are produced in both stroke volume and wall thickness in those athletes that emphasize isometric and weight-bearing exercise.25
In turn, physical exercise reduces resting heart rate, a phenomenon directly related to the increase in stroke volume. This reduction is also apparent during physical exercise in trained individuals when training is done at submaximal intensities. One of the main mechanisms of bradycardia is regulation of the autonomic nervous system, via an increase in vagal tone, although other mechanisms include a decrease in the intrinsic rate of the heart itself, variations in baroreceptor sensitivity, an increase in stroke volume, and, obviously, each individual's genetic makeup.
Another typical and beneficial adaptation caused by exercise is improved coronary circulation, which is partly due to the phenomenon of capillarization. Capillarization consists of an increase in capillary density (number of capillaries per myofibril) and is proportional to the thickening of the myocardial wall, with a consequent increase in coronary blood flow. Moreover, resistance training also increases the diameter of the epicardial coronary vessels26 to maintain adequate perfusion to the increased myocardial mass. Apart from these angiogenesis-related changes, there are also functional adaptations, such as greater relaxation of small coronary arteries and/or production of nitric oxide from coronary endothelium.
The Athlete's HeartRegular training induces adaptive changes in the heart aimed at improving the performance of the cardiovascular system during exercise. This adaptation can increase cardiac mass by up to 20%.17 However, upon clear identification of the possibility of exercise-related heart disease, such as arrhythmias or cardiac arrest, 3 clear research objectives have emerged: a) understanding how cardiac adaptation to exercise can improve athletic ability; b) guiding training to optimize cardiac adaptation, and c) differentiating between normal and pathological cardiac adaptation.24 This latter aspect has generated great interest inside and outside the field of cardiology due to its important preventive and even legal implications.
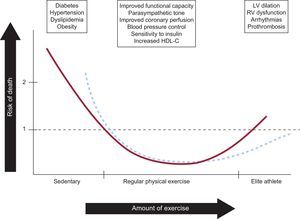
As discussed above, regular physical exercise causes morphological and electrical cardiac remodeling that induces physical adaptation to the cardiac overload promoted by exercise. However, as with many other biological variables, the relationship seems to show a “J curve” distribution, because excessive remodeling, particularly structural, is closely linked to the main serious cardiac diseases related to sport.27 Thus, the major challenge for professionals involved in observing athletes is to identify when cardiac adaptation to exercise starts to pose a risk. However, pathological cardiac adaptation to exercise only occurs in a small percentage of athletes.24,25,28 Accordingly, the challenge for sports cardiologists is to identify previously healthy people that undergo pathological cardiac adaptation during exercise and that have a higher risk of serious cardiac complications.
Cardiac RehabilitationCardiac rehabilitation encompasses a series of coordinated and multidisciplinary interventions that aim to improve the functional capacity, both physical and psychological, of patients with some type of cardiac condition; moreover, it stabilizes and delays the development of the underlying disease, improving its prognosis.29 The main aims of cardiac rehabilitation are to prevent the incapacity produced by cardiovascular diseases and new atherosclerotic complications. Patients also achieve higher rates of smoking cessation and improve their dietary habits.30 Candidate patients for starting cardiac rehabilitation programs are those that have had a myocardial infarction or have angina or heart failure.31
The first cardiac rehabilitation units were founded at the end of the 1960s, and these units have consistently shown effectiveness in reducing mortality by around 25%.30,32–34 There have been considerable advances in cardiac rehabilitation in recent years, progressing from continuous work at programmed and controlled low intensities to complex training programs that, in addition to aerobic exercise, include interval training (combinations of high and low intensity) and strength training.35,36 This approach is used not only because these types of exercises are useful in improving cardiac function, but also because understanding of the physiology of these patients is constantly improving, revealing that their functional limitation is not only a cardiac problem, but is also influenced by many peripheral factors.37 Moreover, work to improve the functional capacity of a patient with heart disease should be maintained, with these programs underpinning and supporting the acquisition of the habit of regular physical exercise.
Effects Beyond the Cardiovascular SystemDespite the physiological adaptations produced, it is of the utmost importance to remember that the most important positive effects of physical exercise are produced not only in the cardiovascular system but also in psychological and sociological aspects and in specific diseases. Consequently, physical activity and exercise are of great importance for treating and preventing cardiovascular risk factors, for almost the entire population.
One of the most direct effects of physical exercise is a reduction in insulin resistance, since exercise increases the glucose uptake ability of muscle tissue. Regular physical activity decreases the risk of type 2 diabetes mellitus.38 In patients with established type 2 diabetes mellitus, physical exercise helps to control blood glucose levels and can sometimes even reduce the need for antidiabetic drugs and/or insulin.5 Habitual physical exercise, even at moderate intensities, decreases insulin resistance in peripheral tissues, improves glucose uptake by skeletal muscle and glycogen metabolism, decreases postprandial hyperglycemia, and helps to reduce body weight, all of which have beneficial effects on glucose control and lower glycated hemoglobin in the medium term. In the classic Diabetes Prevention Program study, a lower incidence of diabetes mellitus during follow-up was seen in patients included in the treatment branch, which involved modification of the patients’ diet and lifestyle.39 Interestingly, the main difference between patients in the treatment and placebo or metformin branches was that the former performed up to 4 times as many hours of physical exercise a week.
Exercise programs with a high dynamic component prevent hypertension and decrease blood pressure, both in normotensive adults and in those with hypertension. This effect is more pronounced in hypertensive patients, with a mean reduction of between 6 mmHg and 7mmHg in systolic and diastolic pressures vs 3mmHg in normotensive patients.40 Regular training reduces resting sympathetic activity, but also decreases the plasma catecholamine concentration (at rest and during submaximal exercise) and modifies renal homeostasis (decrease in renal vascular resistance), all of which help to lower blood pressure.
Physical training plays a fundamental role in preventing and treating excess weight and obesity, particularly if combined with a low-calorie diet. The continual practice of physical activity helps to reduce body weight, mainly fat percentage, and modifies many of the metabolic alterations underlying the development of cardiovascular risk factors. At the same time, a reduction has been shown in inflammatory markers such as C-reactive protein in overweight and obese people.41
Another of the considerable benefits of regular physical exercise is improved lipid profile, and exercise is one of the few effective strategies for increasing the serum concentration of high-density lipoprotein cholesterol.41,42 Therefore, physical exercise has widespread beneficial effects on the body, cardiovascular system, and risk factors.
Finally, physical exercise also has important effects on the central nervous system. One interesting observation is that its effects are produced in all stages of life, because exercise improves the learning ability of adolescents and has beneficial effects for adult diseases, such as depression, Parkinson disease, and Alzheimer disease.17
For all of these reasons, frequent and regular physical exercise should be recommended to the entire population to guarantee an improvement in the quality of life of individuals and also in their physical, psychological, and social states. Equally, some type of supervision of physical exercise is sometimes required, due to both exercise intensity and each person's individual characteristics.
SAFETY IN SPORTImproved reporting and awareness of sports-related deaths and cardiac arrests have generated a growing concern over safety during physical activity. Sudden death is the most serious event that can occur during physical activity and poses the greatest preventive challenge for professionals who recommend physical exercise and who supervise athletes. A suggested representative diagram of the relationship between the amount of exercise and the risk of cardiovascular disease or serious cardiovascular complications is shown in Figure 2. Screening of athletes or people about to begin regular physical exercise is fundamentally aimed at identifying those persons that could have a higher risk of exercise-associated complications. In those < 35 years, the main source of risk is congenital heart disease with structural or electrical alterations43; however, there are many more possibilities in persons older than this age, principally ischemic heart disease and poor cardiac adaptation. Thus, screening before incorporation into physical activity programs and monitoring of athletes with high training loads can identify those individuals with a high risk of complications, which can be prevented by individualized approaches (Figure 2, dotted line).
Association between the amount of exercise and risk of death. The main factors that determine how each level of exercise influences each risk are summarized in the upper squares. The dotted lines show the possibility of reducing the risk of death or complications with screening programs and monitoring of athletes with high training loads. HDL-C, high-density lipoprotein cholesterol; LV, left ventricle; RV, right ventricle.
Contemporary registries have revealed that exercise-related cardiac arrest has an incidence of 0.3/100 000 person-years for those < 35 years and of 3.0/100 000 person-years for those > 35 years.44 This incidence is 10 times lower than that of cardiac arrests unrelated to sport. Strikingly, in this extensive Dutch registry, survival after exercise-related cardiac arrest was much higher (around triple) than after non-exercise-related cardiac arrest. More than 50% of cases of sports-related cardiac arrest are produced in sporting installations or public places adapted to the practice of physical exercise and<18% occur during official competitions.44,45
More than 2 million people participate every year in long-distance races in the United States. An observational registry evaluated the incidence of cardiac arrests related to participation in marathons (42.18 km) or half marathons in the United States during a 10–year period, including 10.9 million runners.46 The incidence of cardiac arrest was 0.54/100 000 participants and most arrests were caused by underlying cardiovascular disease, mainly hypertrophic cardiomyopathy or undiagnosed coronary atherosclerosis. More cases were seen in marathons than in half marathons (1.01/100 000 runners vs 0.27/100 000 runners), and men were more commonly affected than women. Of these cardiac arrests, 71% resulted in death (incidence, 0.39/100 000 runners). The main predictors of survival after cardiac arrest were resuscitation maneuvers by witnesses and diagnosis of a heart disease other than hypertrophic cardiomyopathy. Thus, marathons and half marathons have a low associated risk of cardiac arrest and sudden death.
With regard to cardiac rehabilitation programs, a more exhaustive evaluation of functional degree and cardiac condition is recommended, as with patients with high clinical suspicion of myocardial ischemia.47 In all of these cases, attention must be paid to the onset of prodromal symptoms during physical exercise, chiefly chest pain, disproportionate dyspnea or asthenia, gastrointestinal symptoms, dizziness, or headache. These programs are very safe when performed under supervision, and the complications rate is very low (< 1/10 000 patients).29,30,48
The incidence of sudden death or serious complications during physical exercise is so low that the risk-benefit ratio is clearly in favor of the practice of exercise.
CONCLUSIONSSport has a wide variety of beneficial effects on health, many of which are related to protection against cardiovascular diseases.
CONFLICTS OF INTERESTSNone declared.