Atrial fibrillation (AF) is the most common type of cardiac arrhythmia. It is associated with an increased morbidity and mortality, in particular due to a higher thrombo-embolic risk. The clinical benefits of anticoagulant therapy have been demonstrated repeatedly, with a marked reduction in thrombo-embolic events and mortality.1 However, there are several inherent limitations in vitamin K antagonist (VKA) therapy: variability in the effect (related to clinical and genetic factors), drug interactions and interaction with certain foods, need for frequent routine monitoring, etc. Patients with poor anticoagulation control with a VKA, estimated using the time in therapeutic range (TTR), have a higher probability of complications, both thrombo-embolic and hemorrhagic.2 Likewise, a labile international normalized ratio (INR) is associated with an increased bleeding risk. In fact, labile INR is one of the variables included in the HAS-BLED score for major bleeding risk, which is recommended in the current European guidelines on AF.1 Recent studies carried out in Spain found that anticoagulation control was suboptimal in approximately 40% of patients receiving VKAs3; this percentage could be higher in patients starting VKA anticoagulant therapy.
Regarding the novel oral anticoagulants (NOACs), also known as direct-acting oral anticoagulants (DOACs), various pivotal clinical studies have shown a benefit in the primary efficacy endpoint as well as a clear safety benefit, finding a reduction in the rate of intracranial hemorrhage.1,4 Use of NOACs has been approved by the European and Spanish regulatory agencies. However, the Spanish regulatory approval includes several restrictions for use, which are reflected in the therapeutic positioning report UT/V4/23122013, and, in addition, requires authorization for their prescription.5 Patients who cannot attend for blood monitoring of VKAs and patients with a high bleeding risk, high thrombotic risk, or poor anticoagulation control are clear candidates for NOACs. However, the need for authorization is a bureaucratic obstacle that hinders the use of these treatments. In addition, the authorization process can take several days, or more if additional information is required before authorization is granted. This means a delay in starting treatment and the consequent thrombo-embolic risk to the patient. Another important point is the heterogeneity of the authorization criteria between the different autonomous regions of the country, leading to differences in the level of prescribing of this type of drug nationally.
The authorization requirement results in underprescription and delayed prescription of NOACs in patients who, with such drugs, would have fewer events. With this in mind, and taking into account the professional duty to prescribe the best treatment available, the Spanish Society of Cardiology, along with the other signatory scientific societies of this document, propose that the authorization requirement for NOAC prescription be abolished, as it imposes difficulties and limits on their use, primarily in those patients who could clearly benefit clinically from these drugs. The idea of a budgetary restriction in times of economic crisis is a clear mistake; what is expensive is when our patients have a stroke or major bleeding complication. The use of these drugs has been demonstrated to be cost-effective. Anticoagulant treatment must be individualized, choosing the best treatment for each patient and leaving the prescription of the appropriate agent to the judgment of the responsible physician.
After an exhaustive review of the references available, the Spanish Society of Cardiology and the other signatory scientific societies have developed a positioning document,6 with the aim of achieving maximum patient protection, should the requirement for authorization remain. The document includes 7 changes from the current therapeutic positioning report of the Spanish Medicines Agency (UT/V4/23122013), dated 23 December 2013. These changes are described below. Table 1 shows a summary of the proposed changes.
Main Changes to the Therapeutic Positioning Report of the Spanish Society of Cardiology
| Abolish authorization requirement for prescription of these drugs |
|---|
| If authorization requirement is kept in place, the following modifications are suggested: |
| 1. Use of the CHA2DS2-VASc score for estimation of thrombo-embolic risk |
| 2. High bleeding risk |
| 3. High thrombosis risk. A specific example would be the indication in secondary prevention |
| 4. Access to INR results |
| 5. Reduction in the time used for the calculation of time in therapeutic range |
| 6. Prediction of patients at high risk of suboptimal anticoagulation |
| 7. Electrical cardioversion |
INR, international normalized ratio.
The CHA2DS2-VASc scoring system has been demonstrated to better identify those patients who would benefit from oral anticoagulant therapy: patients with a low risk estimated using the old CHADS2 score could have a moderate or even high risk with the CHA2DS2-VASc score.7 Therefore, the new European1 and American8 clinical practice guidelines for AF both strongly recommend the use of this scoring system over the old CHADS2 score. Given that scientific societies recognize the CHA2DS2-VASc as the most suitable for assessing which patients will benefit from oral anticoagulant therapy, we believe that this score should be recommended for use in establishing the indication for oral anticoagulation and for NOACs. Patients with a CHA2DS2-VASc score ≥ 2 should receive an oral anticoagulant agent. This can probably also be recommended for patients with CHA2DS2-VASc = 1 (provided that the score is not due to female sex without additional risk factors).
Surprisingly, in the last therapeutic positioning report on the use of NOACs (UT/V4/23122013) there was no option regarding their prescription in patients who had had a bleeding complication with VKAs.5 However, one of the greatest benefits of NOACs is their superior safety profile.1 All trials on NOACs have demonstrated a reduction in intracranial hemorrhage, which is the most feared complication due to its significant effect on short- and long-term prognosis. Furthermore, they reduce the risk of major bleeding and hemorrhagic stroke.4 Various studies have demonstrated that the net benefit is greater with NOACs than with VKAs in patients with a high bleeding risk.9 Therefore, it seems reasonable to suggest that patients with a high bleeding risk, which can be estimated by a HAS-BLED score > 3, be candidates for NOACs.
Some studies have demonstrated a greater benefit from NOACs in patients with a high thrombo-embolic risk.10 Therefore, it seems reasonable to suggest that patients with high thrombo-embolic risk, with a CHA2DS2-VASc score > 3, be candidates for NOACs. Importantly, secondary prevention, that is, patients who have already had an embolic stroke, is a situation of fundamentally high thrombo-embolic risk. We completely support the recommendation to use NOACs in patients requiring secondary prevention.
In recent years, interest has grown in the quality of oral anticoagulation. Both the European and the American guidelines,1,8 and more recently the British NICE guidelines,11 make a clear recommendation to achieve optimal anticoagulation. A cutoff point is given for the optimal value of TTR of > 70% in the European guidelines and > 65% in the NICE guidelines. The current therapeutic positioning of the Spanish Medicines Agency (UT/V4/23122013) also stresses the need for optimal anticoagulation, with a TTR of > 65%. Switching to NOACs is indicated for patients with a TTR < 65% when calculated using the Rosendaal method or < 60% for the absolute INR percentage. The Spanish Medicines Agency requires an evaluation period of at least 6 months, excluding INR values from the first month of treatment.5 Frequently, however, patients’ INR results are not available. On some occasions, when it is possible to see the most recent results, only the 3 most recent values are available. Therefore, in the document by the Spanish Society of Cardiology, the authors call for the necessary measures to be taken to ensure ease of access to at least the last 6 INR measurements for any physician attending a patient with AF.6
There is evidence of increased risk of thrombo-embolic and hemorrhagic complications in the months after starting anticoagulant therapy.12 There is also evidence of an increased risk of anticoagulation interruption in this period, which is associated with a higher rate of events.13 Therefore, it seems reasonable to suggest that the TTR evaluation period be shortened to 3 months. In addition, if in the first 3 months there is a poor quality of anticoagulation or inadequate dose adjustment, such patients should be candidates for NOACs.
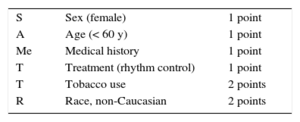
To predict which patients have a higher risk of poor anticoagulation control with VKAs, new methods have been proposed, such as the SAME-TT2R2 score,14 which is based on clinical variables. The scoring system is shown in Table 2. Recently, this score was validated in the Spanish population by various groups. A good correlation was demonstrated between the score and TTR value and the associated occurrence of events during follow-up of patients treated with VKAs. Specifically, the score was demonstrated to prospectively predict anticoagulation quality in patients in Spain on acenocoumarol therapy.14 Therefore, we believe that it would be highly recommendable, before starting anticoagulation with oral AVKs, to identify those patients with a higher probability of suboptimal anticoagulation, which is clearly associated with an increased rate of thrombo-embolic and hemorrhagic events.2 Given that improving anticoagulation quality has been demonstrated as enormously cost-effective,15 it seems reasonable to suggest that patients with a SAMe-TT2R2 score > 2, that is, patients with a high probability of having suboptimal anticoagulation, be candidates for receiving NOACs as the initial anticoagulant therapy. In fact, some autonomous communities of Spain have already adopted this score as part of the authorization for NOAC prescription.
SAME-TT2R2 Score for Predicting the Quality of Oral Anticoagulation
| S | Sex (female) | 1 point |
| A | Age (< 60 y) | 1 point |
| Me | Medical history | 1 point |
| T | Treatment (rhythm control) | 1 point |
| T | Tobacco use | 2 points |
| R | Race, non-Caucasian | 2 points |
*Defined as at least 2 of the following conditions: hypertension, diabetes mellitus, coronary artery disease/myocardial infarction, peripheral vascular disease, heart failure, previous stroke, lung disease, liver disease, or kidney disease.
Electrical cardioversion of AF requires anticoagulation with an INR range of 2.0 to 3.0 in the weeks prior to the procedure.1 Frequently, however, obtaining a stable anticoagulation level can take several weeks. This leads to a delay in cardioversion and undesirable resource use. It has been demonstrated that NOACs are as effective and safe as VKAs in preventing the occurrence of emboli in electrical cardioversion.16,17 The use of NOACs in patients who are scheduled to undergo electrical cardioversion would facilitate scheduling, as it would reduce the delay until the procedure. Therefore, it seems reasonable to suggest that patients who are candidates for cardioversion should be allowed to receive a NOAC before the procedure and for 1 month after.
The Spanish Society of Cardiology has held a round of contacts with several other scientific societies. We should be pleased with this document, because 5 other scientific societies agreed in their support of it: the Spanish Thrombosis and Hemostasis Society (SETH), the Spanish Society of Neurology (SEN), the Spanish Society of Internal Medicine (SEMI), the Spanish Society of Emergency Medicine (SEMES), and the Spanish Society of Primary Care Physicians (SEMERGEN). This initiative confirms the firm opinion of these 6 scientific societies that patients deserve better antithrombotic treatment, and that this should be available for selection on an individual basis. This is not only about using NOACs; it is about ensuring that each patient receives the most appropriate treatment, with the fewest administrative restrictions possible and in line with the scientific evidence, based on their clinical characteristics and thrombo-embolic and hemorrhagic risk, thus reducing as far as possible the risk of complications and improving patients’ prognosis and quality of life.
CONFLICTS OF INTERESTNone declared.