The new, recently published, US guidelines on high blood pressure (BP)1 incorporate important changes to clinical practice that call for reflection. In the first place, it is surprising to see the authors describe the guideline as an update to The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7), as if the JNC-8 had never existed. It would appear that the authors no longer endorse the relaxation of BP goals introduced in the JNC-8.
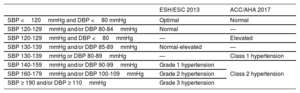
The first major change in the US guideline is the new BP classification system, which is, according to the authors, based on both an analysis of cardiovascular risk and data from clinical trials.1 The most significant modification is in the definition of hypertension, which is now systolic BP (SBP) ≥130 and diastolic BP (DBP) ≥80mmHg, down from the previous levels of SBP ≥140mmHg and DBP ≥90mmH. Obviously, with this change, many individuals previously considered normotensive are now considered hypertensive.2 Nonetheless, during the presentation of the guidelines at the American Heart Association meeting, the authors stated that this new definition of hypertension would not necessarily lead to a surge in the prescription of antihypertensive drugs, as most new hypertensive patients would probably have a low risk of cardiovascular disease and the threshold for initiation of pharmacologic therapy remained unchanged at 140/90mmHg. Another core concept in the new guidelines is the emphasis on the importance of promoting lifestyle change. We cannot help but wonder, however, what benefit there is in telling a patient with a low risk of cardiovascular disease that they now have class I hypertension (SBP 130-139mmHg/DBP 80-89mmHg) and an increased risk of a cardiovascular event, but that we are not going to prescribe them BP-lowering medication because this will have no clinical benefit unless their pressure rises higher? Would it not have been better to leave the definition as it was and emphasize the need for lifestyle change in borderline patients on the verge of hypertension? Applying a similar rationale to those applied in the guidelines, why not lower the glycohemoglobin level defining diabetes from 6.5% to 6.0% or, in the case of dyslipidemia, the low-density lipoprotein cholesterol threshold to <100mg/dL or even better <70mg/dL? Obviously, risk factors are continuous variables and the higher they are, the greater the risk. While this is true, it is also important to establish a threshold after which a given treatment will be beneficial. An additional problem with the new US BP classification is that depending on which guidelines are used (Table 1),1,3 the definition of hypertension will vary in both the literature and clinical practice, causing potential confusion.
Definition of Hypertension According to the 2013 European and the 2017 American Hypertension Guidelines
| ESH/ESC 2013 | ACC/AHA 2017 | |
|---|---|---|
| SBP <120mmHg and DBP <80 mmHg | Optimal | Normal |
| SBP 120-129mmHg and/or DBP 80-84mmHg | Normal | — |
| SBP 120-129mmHg and DBP <80mmHg | — | Elevated |
| SBP 130-139mmHg and/or DBP 85-89mmHg | Normal-elevated | — |
| SBP 130-139mmHg or DBP 80-89mmHg | — | Class 1 hypertension |
| SBP 140-159mmHg and/or DBP 90-99mmHg | Grade 1 hypertension | Class 2 hypertension |
| SBP 160-179mmHg and/or DBP 100-109mmHg | Grade 2 hypertension | |
| SBP ≥ 190 and/or DBP ≥ 110mmHg | Grade 3 hypertension |
The new US guidelines emphasizes the (undeniable) importance of accurate BP measurement, and even provides practical recommendations for this.1 In addition, it stresses the importance of home and ambulatory BP monitoring. Out-of-office measurements are essential for detecting white coat and masked hypertension and are very useful for improving clinical management strategies. The new guideline contains some very practical algorithms for dealing with both white coat and masked hypertension.1
The guidelines also provide some highly useful recommendations for diagnosing and treating secondary forms of hypertension. The authors examine the most common causes of secondary hypertension and review the treatments available. Approximately 10% of all cases of hypertension have a resolvable or at least a treatable cause.1
Substantial changes have been made to BP targets, one of the cornerstones of hypertension treatment. The general target has been lowered from <140/90mmHg to <130/80mmHg. Nonetheless, all hypertensive patients should be advised to undertake lifestyle changes, and drug therapy should only be initiated after assessing cardiovascular risk in addition to baseline BP. In the case of patients with established cardiovascular disease and an estimated 10-year atherosclerotic cardiovascular disease risk of ≥10% or patients with specific comorbidities, such as diabetes, chronic kidney failure, heart failure, ischemic heart disease, or peripheral heart disease, drug therapy should be initiated at 130/80mmHg. The threshold for those without cardiovascular disease and with an estimated 10-year atherosclerotic cardiovascular disease risk <10% or for patients in need of secondary stroke prevention is 140/90mmHg. The threshold for treatment initiation in older patients (≥65 years, noninstitutionalized, ambulatory, community-living adults) is SBP ≥130mmHg, although the goal of <130/80mmHg1 is maintained for all the population. Transferring the US recommendations to Europe is problematic, as the proposed risk stratification scale is not validated for the European population and cannot therefore be applied here. It is also hard to justify why the cutoff for classifying a patient as high risk is 10% for hypertension yet 7.5% for dyslipidemia.1
The new BP control goals in the US guidelines are mainly based on the results of the SPRINT4 and ACCORD5 trials. However, these trials have several particularities that are worth bearing in mind. In the SPRINT trial, although an SPB target of <120mmHg (vs <140mmHg) was associated with a reduction in cardiovascular events, the study did not include important subgroups of patients, such as those with diabetes or a history of stroke, and only 20% of the participants had cardiovascular disease. In addition, intensive BP control was associated with an increased risk of hypotension, syncope, and acute renal failure.4 The second trial, ACCORD, which analyzed patients with type 2 diabetes mellitus and a high risk of a cardiovascular event, did not find intensive BP reduction to be associated with an overall reduction in cardiovascular events.5 Findings from recent meta-analyses have also cast doubts on the potential benefits of intensive BP therapy. One meta-analysis of 76 clinical trials involving 306 273 participants found that lowering of BP was associated with a reduced risk of death and cardiovascular disease in patients with SBP ≥140mmHg. The reduction, however, had no primary prevention benefit in patients with BP below this level, except perhaps in a subgroup of patients with ischemic heart disease.6 A second meta-analysis of 49 clinical trials involving 73 738 participants with type 2 diabetes mellitus found that antihypertensive treatment reduced cardiovascular morbidity and mortality only in patients with baseline SBP >140mmHg, and the findings even suggested that antihypertensive treatment might be harmful in patients with lower levels.7 In brief, different studies have reported controversial, and at times contradictory, results for BP targets.
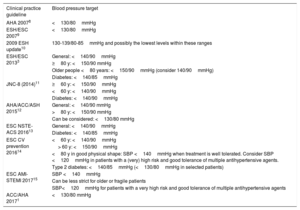
Recommendations on BP goals have varied over the last decade depending on how the evidence available at the time has been analyzed or interpreted, and there have even been variations in the absence of new evidence. Changes in recommended BP targets for patients with ischemic heart disease between 2007 and 2017 are shown in Table 2.1,2,8–15 The target in 2007 was <130/80mmHg but this was subsequently relaxed, mainly for 2 reasons: first, a lack of evidence for a benefit for intensive BP control in this population, and second, the likely existence of a J-curve, whereby intensive lowering of BP could have harmful effects, particularly in more frail populations. This trend, however, appears to have been reversed again with the emergence of new evidence, mostly from the SPRINT trial.
Changes in Blood Pressure Targets for Patients With Ischemic Heart Disease
| Clinical practice guideline | Blood pressure target |
|---|---|
| AHA 20078 | <130/80mmHg |
| ESH/ESC 20079 | <130/80mmHg |
| 2009 ESH update10 | 130-139/80-85mmHg and possibly the lowest levels within these ranges |
| ESH/ESC 20133 | General: <140/90mmHg |
| ≥80 y: <150/90 mmHg | |
| Older people <80 years: <150/90mmHg (consider 140/90mmHg) | |
| Diabetes: <140/85mmHg | |
| JNC-8 (2014)11 | ≥60 y: <150/90mmHg |
| <60 y: <140/90mmHg | |
| Diabetes: <140/90mmHg | |
| AHA/ACC/ASH 201512 | General: <140/90 mmHg |
| >80 y: <150/90 mmHg | |
| Can be considered: <130/80 mmHg | |
| ESC NSTE-ACS 201613 | General: <140/90mmHg |
| Diabetes: <140/85mmHg | |
| ESC CV prevention 201614 | <60 y: <140/90mmHg |
| > 60 y: <150/90mmHg | |
| <80 y in good physical shape: SBP <140mmHg when treatment is well tolerated. Consider SBP <120mmHg in patients with a (very) high risk and good tolerance of multiple antihypertensive agents. | |
| Type 2 diabetes: <140/85mmHg (<130/80mmHg in selected patients) | |
| ESC AMI-STEMI 201715 | SBP <140mmHg |
| Can be less strict for older or fragile patients | |
| SBP<120mmHg for patients with a very high risk and good tolerance of multiple antihypertensive agents | |
| ACC/AHA 20171 | <130/80 mmHg |
ACC, American College of Cardiology; AHA, American Heart Association; AMI-STEMI, acute myocardial infarction with ST-segment elevation; ASH, American Society of Hypertension; CV, cardiovascular; ESC, European Society of Cardiology; ESH, European Society of Hypertension; JNC, Joint National Committee; NSTE-ACS, non-ST-elevation acute coronary syndrome; SBP, systolic blood pressure.
Original table created using data from Whelton et al.,1 Mancia et al.,3,9,10 Rosendorff et al.,8,12 James et al.,11 Roffi et al.,13 Piepoli et al.,14 and Ibanez et al.15
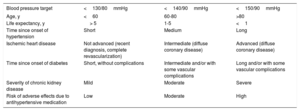
While highly relevant, evidence from clinical trials has serious limitations in that it is based on the application of strict inclusion and exclusion criteria that make it difficult to generalize findings. Considering this limitation, it would probably be better to use individual rather than universal BP targets.16 A 50-year-old patient with single-vessel heart disease who has undergone complete revascularization, for example, is not the same as an 80-year old patient with diffuse coronary artery disease. In the first case, intensive BP control would probably lead to a reduction in cardiovascular events without significantly increasing the risk of adverse effects, while in the second case, the same treatment would probably have a smaller benefit but it would be accompanied by an increased risk of adverse effects. In our opinion, BP targets should be tailored to the clinical characteristics of each patient following an integrated risk assessment (Table 3), as occurs, for example, in patients with diabetes.16
Blood Pressure Targets According to Clinical Characteristics of Patient
| Blood pressure target | <130/80mmHg | <140/90mmHg | <150/90mmHg |
|---|---|---|---|
| Age, y | <60 | 60-80 | >80 |
| Life expectancy, y | > 5 | 1-5 | <1 |
| Time since onset of hypertension | Short | Medium | Long |
| Ischemic heart disease | Not advanced (recent diagnosis, complete revascularization) | Intermediate (diffuse coronary disease) | Advanced (diffuse coronary disease) |
| Time since onset of diabetes | Short, without complications | Intermediate and/or with some vascular complications | Long and/or with some vascular complications |
| Severity of chronic kidney disease | Mild | Moderate | Severe |
| Risk of adverse effects due to antihypertensive medication | Low | Moderate | High |
Original table created using data from Barrios et al.16
The 2017 US guidelines place particular emphasis on lifestyle modifications, primarily dietary changes (low-salt and a Mediterranean-like diet), weight loss, and regular exercise. As mentioned, decisions on pharmacologic treatment should be based on a joint assessment of baseline BP and risk of cardiovascular disease. The guidelines, like earlier versions, establish thiazide-type diuretics as the first-line treatment for patients without special conditions, but it also mentions calcium channel blockers, angiotensin converting enzyme inhibitors, and angiotensin II receptor blockers.1 Once again, and unlike the European guidelines for hypertension management,3 it does not recommend beta-blockers. It recognizes that most patients will need a combination of at least 2 antihypertensive drugs to achieve their BP control goals, but also acknowledges that not all combinations appear to be equally effective. To date, however, just 1 combination, that of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers, has been found to be potentially harmful.1
Finally, the guideline provides specific recommendations on hypertension treatment for patients in special situations or with certain comorbidities (eg, ischemic heart disease, heart failure, pregnancy, children/adolescents, resistant hypertension) and also proposes strategies for improving BP control, which is far from optimal.1 Greater standardization across guidelines, together with more feasible and better defined BP targets, could help to improve control rates. It is difficult to understand how guidelines can offer such different interpretations of the same evidence when it comes to recommending BP goals, and even, as we have seen, defining hypertension. We hope that the forthcoming 2018 guidelines of the European Society of Hypertension and the European Society of Cardiology will shed more light on the most appropriate treatments for hypertension.
Conflicts of InterestNone declared.
.