Delirium is an acute organic brain syndrome characterized by a global deterioration of cognitive functions as a consequence of acute somatic disease.1 It has been found that 10% to 56% of elderly patients can experience delirium during hospitalization, and in Spain its prevalence in patients in nonsurgical services is 25%.1 Acute heart failure (AHF) is a frequent diagnosis in emergency department (ED) patients,2 who often have predisposing factors for delirium, such as comorbidity and biochemical parameters.3 However, less is known about the parameters external to the patient that could lead to the development of delirium. Therefore, the main objective of this study was to analyze the impact of attendance times in the ED on the development of delirium in patients with AHF admitted to a hospitalization ward.
We retrospectively analyzed 750 patients with AHF admitted to the hospitalization ward of a tertiary hospital. We excluded 54 patients who developed delirium in the ED. Upon admission to the hospitalization ward, all patients underwent an initial interview to detect delirium using the reduced Confusion Assessment Method (CAM).4 The CAM instrument comprises 4 items. It has been validated for the diagnosis of delirium, and has high sensitivity (94%-100%) and specificity (90%-95%). Delirium is based on 2 primary manifestations (acute onset and fluctuating course, and inattention) and 2 secondary manifestations (disorganized thinking and altered level of consciousness). The diagnosis of delirium requires the presence of both primary manifestations and at least 1 of the secondary manifestations.4 Demographic, clinical, blood, and time data were collected. Time data were analyzed according to 3 levels: a) admission time in the ED until specialist consultation to re-evaluate hospital admission; b) time from admission in the ED to admission to an inpatient facility; and c) total hospitalization time. This study was an observational study, and so written informed consent was not considered necessary; nevertheless, at the start of the interview all patients were asked for their verbal consent to data collection.
Demographic and other baseline data were analyzed using basic descriptive statistics. Continuous variables are expressed as mean ± standard deviation under the assumption of a normal distribution and categorical variables are expressed as numbers (percentage). Quantitative variables were compared using the Student t test, and associations between qualitative variables were determined using the Pearson chi-square or Fisher exact test. Multivariable logistic regression analysis was used to identify the variables associated with the development of delirium during hospitalization. Statistical analysis was performed using the SPSS software package version 20 (SPSS Inc., Armonk, New York, United States).
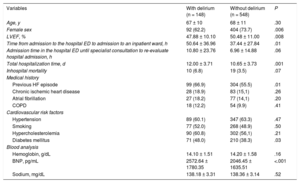
Table 1 shows the characteristics of the study population. Of the 696 patients with AHF admitted to the hospitalization ward, 148 (21.2%) developed primary manifestations at 48hours to 72hours of hospitalization. Group comparisons showed that patients who developed delirium were more frequently male and had a lower left ventricular ejection fraction. The group with delirium had a higher prevalence of a previous medical history of AHF and diabetes mellitus. This group also had higher concentrations of B-type natriuretic peptide at the time of admission to the ED. Finally, this group had longer times from admission to the ED to a hospitalization ward and longer hospitalization times. After adjustment for other covariates, the multivariable analysis showed that time from admission to the ED to admission to a hospitalization ward was an independent predictor of the primary manifestations (Table 2).
Classification of Patients Hospitalized With Heart Failure as a Function of the Development of Delirium During Hospital Admission
| Variables | With delirium (n = 148) | Without delirium (n = 548) | P |
|---|---|---|---|
| Age, y | 67 ± 10 | 68 ± 11 | .30 |
| Female sex | 92 (62.2) | 404 (73.7) | .006 |
| LVEF, % | 47.88 ± 10.10 | 50.48 ± 11.00 | .008 |
| Time from admission to the hospital ED to admission to an inpatient ward, h | 50.64 ± 36.96 | 37.44 ± 27.84 | .01 |
| Admission time in the hospital ED until specialist consultation to re-evaluate hospital admission, h | 10.80 ± 23.76 | 6.96 ± 14.88 | .06 |
| Total hospitalization time, d | 12.00 ± 3.71 | 10.65 ± 3.73 | .001 |
| Inhospital mortality | 10 (6.8) | 19 (3.5) | .07 |
| Medical history | |||
| Previous HF episode | 99 (66.9) | 304 (55.5) | .01 |
| Chronic ischemic heart disease | 28 (18.9) | 83 (15,1) | .26 |
| Atrial fibrillation | 27 (18.2) | 77 (14,1) | .20 |
| COPD | 18 (12.2) | 54 (9.9) | .41 |
| Cardiovascular risk factors | |||
| Hypertension | 89 (60.1) | 347 (63.3) | .47 |
| Smoking | 77 (52.0) | 268 (48.9) | .50 |
| Hypercholesterolemia | 90 (60.8) | 302 (56,1) | .21 |
| Diabetes mellitus | 71 (48.0) | 210 (38.3) | .03 |
| Blood analysis | |||
| Hemoglobin, g/dL | 14.10 ± 1.51 | 14.20 ± 1.58 | .16 |
| BNP, pg/mL | 2572.64 ± 1780.35 | 2046.45 ± 1635.51 | <.001 |
| Sodium, mg/dL | 138.18 ± 3.31 | 138.36 ± 3.14 | .52 |
BNP, B-type natriuretic peptide; COPD, chronic obstructive pulmonary disease; ED, emergency department; HF, heart failure; LVEF, left ventricular ejection fraction.
Unless otherwise indicated, data are expressed as No. (%) or mean ± standard deviation.
Independent Predictors of Delirium in Patients Hospitalized for Heart Failure. Multivariable Analysis
| OR (95%CI) | P | |
|---|---|---|
| Left ventricular ejection fraction | 0.97 (0.95-0.98) | .001 |
| Time from admission to the HES to admission to an inpatient ward, h | 1.14 (1.03-1.26) | .01 |
| Total hospitalization time, d | 1.08 (1.03-1.13) | .002 |
| Previous episode of heart failure 1.53 (1.02-2.29) 0.03 | 1.53 (12.2) | .03 |
95%CI, 95% confidence interval; ED, emergency department; OR, odds ratio.
After adjustment for the following variables: age (P = 0.55), sex (P = 0.07), B-type natriuretic peptide (P = 0.058), and presence of diabetes mellitus (P = 0.26).
The data obtained were similar to data on the prevalence of delirium during hospitalization in patients with AHF.5 The novelty of this study is that it is the first to analyze the impact of length of stay in the ED on the development of delirium in patients with AHF admitted to a hospitalization ward.
In many Spanish hospitals, the organizational structure of EDs, particularly during morning shifts, leads to the prioritization of care of patients already admitted or external consultations. This situation hinders the optimal management of stable patients who are candidates for hospital admission.1 The main limitation of the present study is that it is a retrospective observational study conducted in a single hospital, and it therefore suffers from the bias inherent to such studies. However, the results show the need to reduce the length of time from admission to the ED to admission to a hospitalization ward in order to lower the risk of patients developing delirium. Such reductions would decrease total hospitalization times and therefore lead to lower health costs.