The specialty treating patients with heart failure (HF) has a prognostic impact in the hospital setting but this issue remains under debate in the ambulatory environment. We aimed to compare the clinical profile and outcomes of outpatients with HF treated by cardiologists or internists.
MethodsWe analyzed the clinical, electrocardiogram, laboratory, and echocardiographic data of 2 prospective multicenter Spanish cohorts of outpatients with HF treated by cardiologists (REDINSCOR, n=2150) or by internists (RICA, n=1396). Propensity score matching analysis was used to test the influence of physician specialty on outcome.
ResultsCardiologist-treated patients were often men, were younger, and had ischemic etiology and reduced left ventricular ejection fraction (LVEF). Patients followed up by internists were predominantly women, were older, and a higher percentage had preserved LVEF and associated comorbidities. The 9-month mortality was lower in the REDINSCOR cohort (11.6% vs 16.9%; P<.001), but the 9-month HF-readmission rates were similar (15.7% vs 16.9%; P=.349). The propensity matching analysis selected 558 pairs of comparable patients and continued to show significantly lower 9-month mortality in the cardiology cohort (12.0% vs 18.8%; RR, 0.64; 95% confidence interval [95%CI], 0.48-0.85; P=.002), with no relevant differences in the 9-month HF-readmission rate (18.1% vs 17.2%; RR, 0.95; 95%CI, 0.74-1.22; P=.695).
ConclusionsAge, sex, LVEF and comorbidities were major determinants of specialty-related referral in HF outpatients. An in-depth propensity matched analysis showed significantly lower 9-month mortality in the cardiologist cohort.
Keywords
Heart failure (HF) is a leading public health problem, with a rising incidence and prevalence.1 Although effective treatments have been developed in the past 2 decades and have improved patient survival, HF has an adverse prognosis and is the leading cause of hospitalization.2,3 It has been reported that the medical specialty responsible for the care of patients with HF has an impact on survival, but this issue is still controversial and continues to be debated.4–14 Patients with HF are not treated only by cardiologists, but by a broad range of specialists, most particularly, internists and primary care physicians.10,15 Internists tend to treat older patients, most commonly women, with preserved systolic function and more comorbidities.16 Conversely, patients under the care of cardiology tend to be younger, with a history of ischemic heart disease and reduced systolic function, and in more advanced stages of the disease.17 Outpatient follow-up of HF patients plays a crucial role in long-term prognosis, but most previous studies analyzing the influence of the treating medical specialty have been conducted in hospital patients,15 which does not accurately reflect the clinical condition of outpatients.
Therefore, the aim of our study was to analyze the clinical profile, treatment, and prognosis of outpatients with HF according to whether they were attended by a cardiologist or an internist during follow-up.
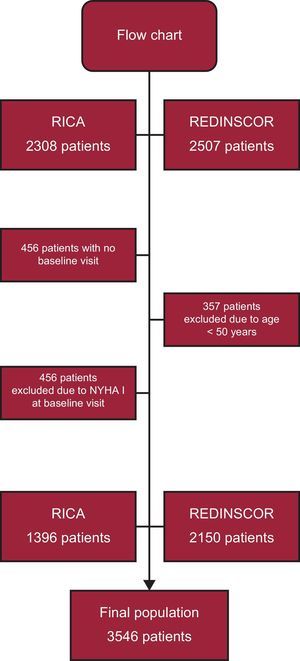
METHODSStudy PopulationThe study was based on a retrospective design with a study population composed of 2 national registries of patients with HF. The first is the REDINSCOR (Red Española de Insuficiencia Cardiaca [Spanish Network for Heart Failure]) registry,, a prospective observational study conducted in HF units at 18 hospitals in Spain that included a total of 2507 outpatients between January 2007 and March 2013 who met the following criteria: age ≥ 18 years, hospitalization for HF in the previous year, and 1 or more of the following echocardiographic abnormalities: left ventricular ejection fraction (LVEF) ≤ 40%, end-diastolic diameter ≥ 60 mm, ventricular relaxation abnormality characteristic of diastolic dysfunction, and interventricular septum and/or posterior wall thickness ≥ 14 mm. Patients were excluded if they had HF secondary to severe valve disease eligible for surgical repair, right HF secondary to chronic cor pulmonale or congenital heart disease, and/or concomitant end-stage disease.
The second registry was the RICA (Registro Nacional de Insuficiencia Cardiaca [National Registry for Heart Failure]), created by the HF Working Group of the Spanish Society of Internal Medicine. This cohort study included 2308 consecutive patients hospitalized for HF from 52 public and private hospitals in Spain between January 2008 and May 2013. The inclusion criteria were age >50 years and HF criteria according to the current guidelines of the European Society of Cardiology.18 The only exclusion criterion was HF secondary to pulmonary hypertension.
Both registries complied with the Declaration of Helsinki, and the respective protocols were approved by the ethics committees at each site. All patients signed an informed consent form.
VariablesClinical data were recorded in electronic forms specifically designed for each registry19,20 with monthly quality controls. The following variables were recorded during inclusion: a) demographic data and patient history; b) information on current illness and physical examination; c) chest X-ray; d) electrocardiogram; e) echocardiogram; f) blood work, and g) drug therapy (Appendix 2 of the supplementary material). Anemia was defined as a hemoglobin value<120 g/L in women and<130 g/L in men. Plasma levels of brain natriuretic peptide and N-terminal pro-B-type natriuretic peptide were dichotomized at cutoff values >150 or >1000 ng/L, respectively. Glomerular filtration rate was estimated using the Chronic Kidney Disease formula.
Record Comparability and Follow-upOutpatient follow-up was performed every 6 months after the inclusion visit in the REDINSCOR registry and at 1, 3, 6, and 12 months after discharge in the RICA registry. To homogenize both populations, the 3-month visit of the RICA registry was taken as the baseline visit comparable to the initial REDINSCOR visit. In addition, REDINSCOR patients aged ≤ 50 years were excluded. Figure 1 shows the flow chart which yielded the final size of our population: 3546 patients (60.4% from cardiology [REDINSCOR] and 39.6% from internal medicine [RICA]). The main events, analyzed separately, were the rate of rehospitalization for HF or any-cause death at 9 months from inclusion. Follow-up data were recorded at each visit and whenever the electronic medical histories were reviewed. The events were validated by an independent data collection committee.
Statistical AnalysisContinuous variables are expressed as the mean ±standard deviation or median [interquartile range] when necessary. The means were compared using the Student t test or the Mann-Whitney U test for independent samples. Categorical variables are expressed as frequencies and percentages, and were compared by the chi-square test or Fisher exact test. P values<.05 were considered statistically significant.
Propensity Score Matched AnalysisTo determine the impact of the medical specialty responsible for the patient on prognosis, propensity score matching21 was performed by binary logistic regression. This procedure introduced the baseline variables which were statistically significant between the 2 cohorts in the bivariable analysis: age, sex, systolic blood pressure, heart rate, New York Heart Association functional class, HF etiology, history of myocardial infarction, anemia, atrial fibrillation, right bundle-branch block, left bundle-branch block, LVEF, estimated glomerular filtration rate<60mL/min/1.73 m2, loop diuretics, beta-blockers, angiotensin-converting enzyme inhibitors, aldosterone receptor antagonists, and aldosterone antagonists. The matched propensity score attempts to neutralize differences between these baseline characteristics for both groups.22 In this case, the 1:1 protocol was used without replacement, using a caliper width of 0.2 standard deviations for the propensity score using the nearest neighbor matching method. To confirm the matching result, the standard difference was used between the means of the continuous and binary variables because it was not influenced by the sample size and allows comparison of the relative balance of the variables with different units.23 The analyses were performed with SPSS 22 and the MatchIt24 statistical package for R 3.2.
RESULTSTable 1 shows the main clinical and treatment differences of HF patients between the 2 registries.
Clinical Characteristics of the Study Population
| RICA (n=1396) | REDINSCOR (n=2150) | P | |
|---|---|---|---|
| University hospital | 897 (64) | 2150 (100) | <.001 |
| Physical examination findings | |||
| Age, y | 78.9 ± 8.3 | 69.7 ± 10.0 | <.001 |
| Women | 757 (54) | 677 (31) | <.001 |
| BMI | 27.7 (24.7-31.9) | 28.1 (25.4-31.2) | .246 |
| Systolic BP, mmHg | 130 (115-143) | 120 (110-135) | <.001 |
| HR, bpm | 75 (67-84) | 74 (65-84) | .066 |
| NYHA class III-IV | 451 (32) | 1253 (58) | <.001 |
| Etiology of HF | |||
| Ischemic | 378 (30) | 1085 (50) | <.001 |
| Hypertensive | 537 (42) | 283 (13) | <.001 |
| Valve disease | 244 (19) | 173 (8) | <.001 |
| Comorbidities | |||
| Smoker | 89 (9) | 294 (14) | <.001 |
| Diabetes mellitus | 633 (45) | 959 (45) | .710 |
| Hypertension | 1233 (88) | 1538 (72) | <.001 |
| Dyslipidemia | 672 (48) | 1199 (56) | <.001 |
| History of myocardial infarction | 87 (7) | 852 (40) | <.001 |
| Peripheral vascular disease | 168 (12) | 299 (14) | .068 |
| Obesity | 416 (35) | 725 (34) | .535 |
| Anemia | 698 (50) | 877 (41) | <.001 |
| Renal failure (eGFR <60 mL/min/1.73 m2) | 871 (62) | 954 (44) | <.001 |
| Electrocardiography | |||
| Sinus rhythm | 510 (37) | 1332 (63) | <.001 |
| Atrial fibrillation | 783 (56) | 561 (26) | <.001 |
| RBBB | 175 (13) | 220 (10) | <.047 |
| LBBB | 268 (19) | 510 (24) | <.001 |
| Echocardiography | |||
| LVEF, % | 53 (40-62) | 33 (25-42) | <.001 |
| LVEF >45% | 845 (63) | 438 (21) | <.001 |
| LA size, mm | 47 (42-52) | 47 (42-53) | .526 |
| LVEDD, mm | 51 (44-58) | 60 (53-67) | <.001 |
| LVESD, mm | 37 (30-48) | 48.0 (40-56) | <.001 |
| Blood work | |||
| Hemoglobin, mg/dL | 12.3 (11.1-13.5) | 13.0 (11.7-14.4) | <.001 |
| Creatinine, mg/dL | 1.2 (1.0-1.6) | 1.1 (0.9-1.4) | <.001 |
| eGFR, mL/min/1.73 m2 | 52 (38-69) | 63 (47-81) | <.001 |
| Potassium, mEq/L | 4.5 (4.1-4.9) | 4.4 (4.1-4.8) | .007 |
| Sodium, mEq/L | 140 (138-142) | 139 (137-142) | <.001 |
| Sodium <135 mEq/L | 134 (10) | 238 (11) | .151 |
| BNP, ng/L | 368 (190-902) | 268 (136-539) | .002 |
| NT-proBNP, ng/L | 2072 (834-4436) | 1782 (748-4531) | .257 |
| BNP >150 ng/L or NT–proBNP >1000 ng/L | 361 (92) | 1516 (100) | <.001 |
| Positive troponin | 97 (20) | 446 (25) | .009 |
| Drug therapy | |||
| Loop diuretics | 1267 (91) | 1820 (85) | <.001 |
| Beta-blockers | 874 (63) | 1681 (78) | <.001 |
| ACE inhibitors | 652 (47) | 1370 (64) | <.001 |
| ARBs | 426 (31) | 484 (23) | <.001 |
| Aldosterone antagonists | 448 (32) | 1160 (54) | <.001 |
| Antiplatelet agents | 364 (26) | 598 (28) | .241 |
| Anticoagulants | 633 (45) | 681 (32) | <.001 |
| Optimal medical treatment* | 239 (17) | 840 (39) | <.001 |
ACE, inhibitor, angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; BMI, body mass index; BNP, pro-brain natriuretic peptide; BP, blood pressure; eGFR, estimated glomerular filtration rate; HF, heart failure; HR, heart rate; LA, left atrium; LBBB, left bundle-branch block; LVEDD, left ventricular end-diastolic diameter; LVESD, left ventricular end-systolic diameter; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal part of pro-B-type natriuretic peptide; NYHA, New York Heart Association functional class; RBBB, right bundle-branch block.
Data are expressed as No. (%) or mean ±standard deviation or median (range).
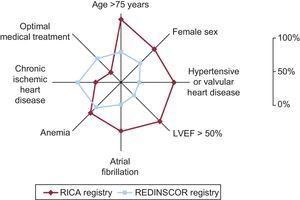
Patients treated by cardiologists (REDINSCOR) were younger, more likely to be male, and had worse New York Heart Association functional class than those followed up by internists (RICA). The main cause of HF was ischemic in the cardiological cohort and valvular and hypertensive in the cohort of patients followed up by internists. Comorbidities, such as hypertension, atrial fibrillation, anemia, or renal failure were significantly more common in the RICA cohort. The physical examination showed almost no differences between the 2 groups in body mass index, heart rate, or systolic blood pressure values. Figure 2 illustrates the typical clinical profile of all patients according to the medical specialty responsible for their care.
Clinical profile of internal medicine and cardiology patients. The figure shows the main clinical differences of patients according to whether they were attended by an internist or a cardiologist. LVEF, left ventricular ejection fraction. Optimal medical treatment: comcomitant prescription of beta-blockers+angiotensin-converting enzyme inhibitors or angiotensin receptor blockers+aldosterone antagonists.
An electrocardiogram and an echocardiogram were performed in more than 95% of patients in both registries. Sinus rhythm was the baseline rhythm in almost 60% of patients under the care of cardiology, whereas atrial fibrillation was the predominant rhythm in patients followed up by internal medicine. Left and right bundle-branch blocks were observed more often in the group followed up by cardiologists. In the REDINSCOR cohort, significantly reduced LVEF predominated (< 35%) whereas preserved LVEF (≥ 50%) was predominant in the RICA cohort. Hemoglobin, creatinine, sodium, potassium, and troponin concentrations were clinically similar in both groups, but estimated glomerular filtration rate was significantly lower in the group under the care of internal medicine. Natriuretic peptides were only determined in 28% of patients attended by internists, but were available in 71% of those followed up by cardiologists (P<.001).
Drug TherapyCardiologists prescribed more beta-blockers, angiotensin-converting enzyme inhibitors, and aldosterone antagonists, whereas internists were more likely to prescribe loop diuretics, angiotensin receptor blockers, and anticoagulants. Optimal medical treatment, considered to be the simultaneous prescription of beta-blockers, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers, and aldosterone antagonists, when indicated, was started more often in the group under the care of cardiology (Table 1).
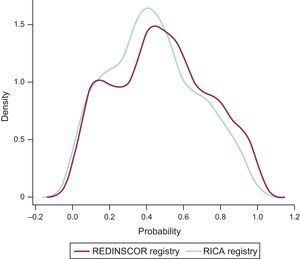
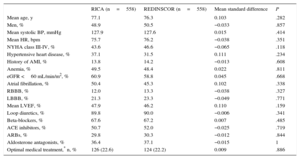
PrognosisPatients attended by cardiology (REDINSCOR) showed a significantly lower 9-month mortality rate (11.6% vs 16.9%; P<.001) than those followed up by internal medicine, with a similar rehospitalization rate for HF (15.7% vs 16.9%; P=.349). After matching patients by baseline variables that were statistically significant in the bivariable analysis between the 2 cohorts, 558 pairs of patients were obtained with similar clinical profiles and electrocardiogram, echocardiogram, and drug therapy characteristics (Table 2). In this selected subgroup, 9-month mortality continued to be lower among patients followed up by cardiology (12.0% vs 18.8%; hazard ratio [HR], 0.64; 95% confidence interval [95%CI], 0.48-0.85; P=.002), with no significant differences in the 9-month rehospitalization rate for HF (18.1% vs 17.2%; HR, 0.95; 95%CI, 0.74-1.22; P=.695) (Table 3). Figure 3 illustrates the extent of propensity score matching in each registry, which highlights the comparability of this selected subgroup.
Clinical Characteristics of the 1:1 Matched Cohort
| RICA (n=558) | REDINSCOR (n=558) | Mean standard difference | P | |
|---|---|---|---|---|
| Mean age, y | 77.1 | 76.3 | 0.103 | .282 |
| Men, % | 48.9 | 50.5 | −0.033 | .857 |
| Mean systolic BP, mmHg | 127.9 | 127.6 | 0.015 | .414 |
| Mean HR, bpm | 75.7 | 76.2 | −0.038 | .351 |
| NYHA class III-IV, % | 43.6 | 46.6 | −0.065 | .118 |
| Hypertensive heart disease, % | 37.1 | 31.5 | 0.111 | .234 |
| History of AMI, % | 13.8 | 14.2 | −0.013 | .608 |
| Anemia, % | 49.5 | 48.4 | 0.022 | .811 |
| eGFR <60 mL/min/m2, % | 60.9 | 58.8 | 0.045 | .668 |
| Atrial fibrillation, % | 50.4 | 45.3 | 0.102 | .338 |
| RBBB, % | 12.0 | 13.3 | −0.038 | .327 |
| LBBB, % | 21.3 | 23.3 | −0.049 | .771 |
| Mean LVEF, % | 47.9 | 46.2 | 0.110 | .159 |
| Loop diuretics, % | 89.8 | 90.0 | −0.006 | .341 |
| Beta-blockers, % | 67.6 | 67.2 | 0.007 | .485 |
| ACE inhibitors, % | 50.7 | 52.0 | −0.025 | .719 |
| ARBs, % | 29.8 | 30.3 | −0.012 | .844 |
| Aldosterone antagonists, % | 36.4 | 37.1 | −0.015 | 1 |
| Optimal medical treatment,* n, % | 126 (22.6) | 124 (22.2) | 0.009 | .886 |
ACE, inhibitor, angiotensin-converting enzyme; AMI, acute myocardial infarction; ARBs, angiotensin receptor blockers; BP, blood pressure; eGFR, estimated glomerular filtration rate; HR, heart rate; LBBB, left bundle-branch block; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional class; RBBB, right bundle-branch block.
Summary of the Gross and Propensity Score-Adjusted Event Rates on Follow-up
| Gross event rate | RICA (n=1396) | REDINSCOR (n=2150) | P |
|---|---|---|---|
| 9-month rehospitalization for HF, n, % | 236 (16.9) | 338 (15.7) | .349 |
| 9-month mortality, n, % | 236 (16.9) | 249 (11.6) | <.001 |
| Adjusted event rate | RICA (n=558) | REDINSCOR (n=558) | P |
|---|---|---|---|
| 9-month rehospitalization for HF, n, % | 96 (17.2) | 101 (18.1) | .695 |
| 9-month mortality, n, % | 105 (18.8) | 67 (12.0) | .002 |
HF, heart failure.
Probability (propensity score) of a patient belonging to the REDINSCOR or RICA registries. Extent of propensity score matching for belonging to the REDINSCOR or RICA registries. The figure depicts considerable consistency between the probability distributions for both groups, which indicates that they are comparable.
The novelty of our study lies in the application of a rigorous matching analysis to determine the influence of the medical specialty in charge—cardiology or internal medicine—on the prognosis of outpatients with HF. For this, 2 national registries of patients with chronic HF were analyzed, the differing clinical profiles were adjusted for each cohort using a complete propensity score, and a lower 9-month mortality rate was found for patients followed up by cardiology.
Influence of Medical SpecialtyA large number of previous studies have shown that the medical specialty responsible for the care of patients with HF is closely related to prognosis.4–14 Although most articles report a more favorable clinical course in patients attended by cardiologists, there are various confounding factors that should be mentioned. In our opinion, the most important is the noticeably different profile of patients historically attended by the 2 specialties. As observed in our study, cardiologists tend to treat patients who are younger, more likely male, with a history of ischemic heart disease, worse functional class, and reduced LVEF. In contrast, internists attend older patients, more often female, and with a higher number of associated comorbidities and usually with preserved LVEF.25–27 In addition to the classic limitation of differing profiles, other studies have collected patients’ clinical variables from administrative databases rather than clinical registries,10,12 which limits the available information on relevant aspects such as treatment or additional tests (eg, lab work, electrocardiography, and echocardiography).5,8,28–30 To compensate for these limitations, a propensity score matching analysis was performed with a series of up to 18 differential baseline variables with prognostic impact on mortality and rehospitalization for HF. The model matched 558 patients from the 2 cohorts, with very similar clinical, analytical, electrocardiographic, echocardiographic, and pharmacological therapy characteristics. Under these conditions, 9-month mortality was significantly lower in patients followed up by cardiologists, with a similar rate of rehospitalization for HF in both cohorts.
The mechanisms for the lower mortality of the REDINSCOR registry are unclear. Patients followed up in the specific HF units at tertiary hospitals may benefit from more comprehensive care and receive a higher number of therapies known to have prognostic benefit, such as cardiac resynchronization, defibrillators, or coronary revascularization.9,31–34 In fact, before patients were included in the study, resynchronization therapy or defibrillators were applied to 16% of REDINSCOR patients compared with 2% of patients in the RICA registry. On the other hand, the higher prescription of optimal medical treatment by cardiologists could theoretically and partially explain the better prognosis of their cohort. However, once the results were adjusted for treatment, the differences in mortality held steady. It is worth mentioning that the total percentage of optimal medical treatment in the study population (37%) is well below recommended levels in the clinical practice guidelines, reflecting the current gap between clinical trial outcomes and real-world daily practice.35–39
Traditionally, internists have followed up patients with HF who require fewer additional tests, such as echocardiography.6,9,11,40 In our study, however, more than 95% of patients treated by internists or cardiologists had an electrocardiogram and echocardiogram performed during follow-up. Conversely, natriuretic peptides were measured less often in patients followed up by internists (28% vs 71%), possibly because many patients had HF with preserved LVEF, and in this subgroup, the benefit of biomarker monitoring has still not been proven.41–45 In addition, the unequal availability of test resources between the hospitals in the RICA registry could be explained by the low percentage of biomarker assays in this cohort.
Last, the volume of patients with HF attended by each specialty and the level of complexity at each hospital facility may have influenced patient prognosis. Recently, this possible effect was analyzed in a large retrospective cohort of patients hospitalized in the United States (n=471 612).12 The authors observed a close relationship between HF-related mortality and physician volume, the medical speciality itself, and hospital complexity. Consequently, the hospitals with higher patient volume and the cardiologists had the best outcomes, which indicates the importance of experience when treating patients with HF. In this regard, the REDINSCOR registry combines 18 hospitals with specific HF units, most of them with a heart transplant program. In contrast, the RICA registry is composed of a more heterogeneous group of 52 public and private hospitals that include tertiary and county hospitals, where the availability of additional tests or complex therapies may be more limited. We could not determine the effect of physician volume on our results because neither registry was designed for this purpose. Nevertheless, this underscores the importance that the medical practitioner responsible for the care of patients with HF receive specific training in this field, irrespective of their medical specialty.
Study LimitationsOur study has several limitations. The first is that patients from the RICA registry were included during a hospital stay. To ensure greater uniformity between the 2 registries, the 3-month visit after discharge was chosen as the baseline visit for comparison with the initial visit in the REDINSCOR registry. However, we believe that, because all REDINSCOR patients had 1 episode of hospitalization for HF in the year prior to inclusion, and because of the 3-month window after the registration of RICA patients, both visits can be considered a reasonable starting point to compare the follow-up of both cohorts. Second, although rigorous matching was performed with 18 variables to neutralize the different clinical profile of patients, the REDINSCOR cohort did not collect relevant information on other comorbidities, such as dementia, lung diseases, or functional status. The latter was an independent predictor of early mortality in the RICA registry.46 In addition, the RICA cohort did not list the exact date associated with each event and, consequently, a survival analysis using Cox regression was impossible. Likewise, specific training in HF among internists was not taken into consideration, and information on drug doses and contraindications was not available in our study. Last, the conclusions drawn are only applicable to the sample of matched patients.
CONCLUSIONSOur study reflects the different clinical profile of outpatients with HF attended by cardiologists and internists in Spain. Whereas patients followed up by cardiology tended to be men, younger, with HF of ischemic etiology, and reduced LVEF, those followed up by internists were predominantly women, older, comorbid, with hypertensive or valvular heart disease, and with preserved LVEF. After close matching, 9-month mortality was significantly lower among patients managed by cardiology, with a similar rate of rehospitalization for HF. This work reinforces the message that the care of patients with HF should be multidisciplinary and that the medical practitioners responsible for their care should receive specific training on the condition.
FUNDINGFunded by the Redes Temáticas de Investigación Cooperativa en Salud [Thematic Networks for Cooperative Research in Health) [RD06-0003-0000] and Red de Investigación Cardiovascular [Cardiovascular Research Network [RD12/0042/0002].
CONFLICTS OF INTERESTNone declared.
- –
The medical specialty responsible for patients hospitalized with HF has a prognostic impact, but this issue is not clear in the outpatient setting. Patients are not treated only by cardiologists, but by a broad range of specialists, mainly internists and primary care physicians.
- –
The prognosis of outpatients with HF attended by cardiologists and internists was analyzed, adjusting for differences between the clinical profile of the 2 groups by using a rigorous propensity score.
To all the investigators and the RICA coordinating center (S&H Medical Science Service) for their statistical and administrative support.