Underuse of beta-blockers has been reported in elderly patients with heart failure. The aim of this study was to evaluate the current prescription of beta-blockers in the internal medicine setting, and its association with morbidity and mortality in heart failure patients.
MethodsThe information analyzed was obtained from a prospective cohort of patients hospitalized for heart failure (RICA registry] database, patients included from March 2008 to September 2011) with at least one year of follow-up. We investigated the percentage of patients prescribed beta-blockers at hospital discharge, and at 3 and 12 months, and the relationship of beta-blocker use with mortality and readmissions for heart failure. Patients with significant valve disease were excluded.
ResultsA total of 515 patients were analyzed (53.5% women), with a mean age of 77.1 (8.7) years. Beta-blockers were prescribed in 62.1% of patients at discharge. A similar percentage was found at 3 months (65.6%) and 12 months (67.9%) after discharge. All-cause mortality and the composite of all-cause mortality and readmission for heart failure were significantly lower in patients treated with beta-blockers (hazard ratio=0.59, 95% confidence interval, 0.41-0.84 vs hazard ratio=0.64, 95% confidence interval, 0.49-0.83). This decrease in mortality was maintained after adjusting by age, sex, ejection fraction, functional class, comorbidities, and concomitant treatment.
ConclusionsThe findings of this study indicate that beta-blocker use is increasing in heart failure patients (mainly elderly) treated in the internal medicine setting, and suggest that the use of these drugs is associated with a reduction in clinical events.
Keywords
Heart failure (HF) is a prevalent condition with high associated morbidity and mortality rates, making it an important health problem, particularly in the elderly population.1–3 In the last decade, there have been substantial advances in pharmacologic treatment for HF caused by systolic dysfunction.4 Nonetheless, HF-related morbidity and mortality remains a concern in clinical practice, above all in elderly patients. To a great extent, this may be due to implementation of insufficient therapy owing to excessive concern about the use of beta-blockers (BB).5 In a previous registry (2002) of the Sociedad Española de Medicina Interna (SEMI, Spanish Society of Internal Medicine), BB use in HF patients was quite low (9.8% overall and 12.3% in systolic HF),6 and in a later study (2006), it reached 35.3%.7
In systolic HF, BB are an essential part of the basic treatment.4 In HF with preserved ejection fraction, there is little available scientific evidence regarding the treatment to use.8–11 Nonetheless, considering the pathophysiologic basis of this condition, BB prescription is widely recommended because of its anti-ischemic, hypotensive, and negative chronotropic actions.4
Based on the data recorded in RICA registry,12 the Spanish HF registry, we evaluated the current status of BB use in hospitalized patients with HF, mainly elderly persons, who were followed up for 1 year in internal medicine departments. Our working hypothesis was that BB are now prescribed more often in this population and that their use is associated with a better clinical evolution. Specifically, the aims of the study were: a) to determine the percentage of patients who receive BB at hospital discharge and at 3 months and 1 year of follow-up, and b) to evaluate the association between BB use and morbidity and mortality.
METHODSPatientsThe patient data were obtained from the information collected in the RICA registry between March 2008 and September 2011. RICA is a prospective multicenter cohort registry coordinated by the SEMI Working Group on Heart Failure.13,14 Briefly, it includes patients hospitalized for an episode of decompensated HF, consecutively attended by the physicians participating in the study. In the event that a case was not entered in the registry, it was not because of any inherent characteristic of the patient. The data were filled in using a web site12 and anonymized to ensure patient confidentiality. Data were analyzed at the time of inclusion (hospital discharge) and at 3 and 12 months of follow-up. The registry includes data from 52 public health and private hospitals providing different levels of medical care. The study protocol was approved by the Ethics Committee of Hospital Universitario Reina Sofía de Córdoba, and informed consent was obtained from all patients before enrollment in the study.
Inclusion CriteriaIn addition to providing informed consent, patients had to be older than 50 years and have been admitted for decompensated HF according to the criteria of the European Society of Cardiology15: a) presence of HF symptoms; b) objective evidence of cardiac dysfunction (systolic or diastolic), preferably by echocardiography, and c) in cases of an inconclusive diagnosis, an adequate clinical response to HF treatment.
Exclusion CriteriaPatients with HF secondary to pulmonary hypertension and those who refused to participate were not included in the study. In addition, we excluded patients with significant valvular dysfunction (moderate-severe or severe), and analyzed only those patients with at least 1 year of follow-up.
Study VariablesAt the time patients were included, we recorded the following data: a) sociodemographic variables (age, sex); b) clinical history and characteristics (hypertension, diabetes mellitus, smoking, acute myocardial infarction, atrial fibrillation, hyperlipidemia, chronic obstructive pulmonary disease, neoplasm, peripheral arterial disease, stroke, Charlson comorbidity index,16 previous functional capacity evaluated with the Barthel index17 before the decompensation that required admission, blood pressure, heart rate, and New York Heart Association [NYHA] functional class); c) analytical data (renal function, hemoglobin and natremia); d) electrocardiographic and echocardiographic parameters (branch block, left ventricular hypertrophy, and left ventricular ejection fraction [LVEF], considered to be preserved at more than 50%), and e) treatment (BB, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, aldosterone antagonists, diuretic, digoxin, statin, dicoumarin, and acetylsalicylic acid).
During follow-up, information was obtained on overall mortality and hospital readmissions for HF. Patients were analyzed in 2 groups, according to whether or not they received BB.
Statistical AnalysisQualitative variables were analyzed using the chi-square test and quantitative variables with the Student t test. Survival analyses were performed with Kaplan-Meier curves. Comparisons of survival curves were carried out with the log rank test. Multivariate analysis using Cox proportional hazards regression models was carried out, including variables that were statistically significant in the univariate model and those considered to have prognostic value regardless of their statistical significance. The level of significance was established at P<.05. All statistical analyses were performed with IBM SPSS, version 20.0.
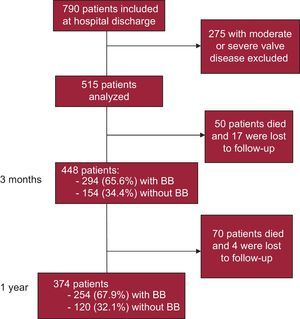
RESULTSPatient Sample AnalyzedThe flow chart of the patients evaluated is shown in Figure 1. In September of 2011, there were 1478 patients in the RICA registry, 790 of whom had reached 1 year of follow-up. From this total, 275 were excluded because of significant valvular disease, which left 515 patients for the analysis. Mean age was 77.1 (8.7) years, and 53.6% were women. At 3 and 12 months following discharge, 50 and 70 patients, respectively, had died, and information was missing in 17 (7 with BB) and 4 (2 with BB) cases, respectively.
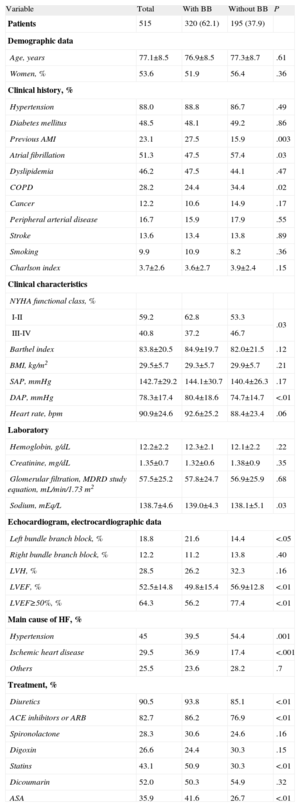
Patient Characteristics at Hospital DischargeThe baseline clinical characteristics at the time of hospitalization and the treatment at discharge in the overall series and in the subgroups with and without BB treatment are shown in Table 1.
Baseline Characteristics at Admission and Treatment at Discharge of Patients With and Without Beta-blocker Treatment
| Variable | Total | With BB | Without BB | P |
| Patients | 515 | 320 (62.1) | 195 (37.9) | |
| Demographic data | ||||
| Age, years | 77.1±8.5 | 76.9±8.5 | 77.3±8.7 | .61 |
| Women, % | 53.6 | 51.9 | 56.4 | .36 |
| Clinical history, % | ||||
| Hypertension | 88.0 | 88.8 | 86.7 | .49 |
| Diabetes mellitus | 48.5 | 48.1 | 49.2 | .86 |
| Previous AMI | 23.1 | 27.5 | 15.9 | .003 |
| Atrial fibrillation | 51.3 | 47.5 | 57.4 | .03 |
| Dyslipidemia | 46.2 | 47.5 | 44.1 | .47 |
| COPD | 28.2 | 24.4 | 34.4 | .02 |
| Cancer | 12.2 | 10.6 | 14.9 | .17 |
| Peripheral arterial disease | 16.7 | 15.9 | 17.9 | .55 |
| Stroke | 13.6 | 13.4 | 13.8 | .89 |
| Smoking | 9.9 | 10.9 | 8.2 | .36 |
| Charlson index | 3.7±2.6 | 3.6±2.7 | 3.9±2.4 | .15 |
| Clinical characteristics | ||||
| NYHA functional class, % | ||||
| I-II | 59.2 | 62.8 | 53.3 | .03 |
| III-IV | 40.8 | 37.2 | 46.7 | |
| Barthel index | 83.8±20.5 | 84.9±19.7 | 82.0±21.5 | .12 |
| BMI, kg/m2 | 29.5±5.7 | 29.3±5.7 | 29.9±5.7 | .21 |
| SAP, mmHg | 142.7±29.2 | 144.1±30.7 | 140.4±26.3 | .17 |
| DAP, mmHg | 78.3±17.4 | 80.4±18.6 | 74.7±14.7 | <.01 |
| Heart rate, bpm | 90.9±24.6 | 92.6±25.2 | 88.4±23.4 | .06 |
| Laboratory | ||||
| Hemoglobin, g/dL | 12.2±2.2 | 12.3±2.1 | 12.1±2.2 | .22 |
| Creatinine, mg/dL | 1.35±0.7 | 1.32±0.6 | 1.38±0.9 | .35 |
| Glomerular filtration, MDRD study equation, mL/min/1.73 m2 | 57.5±25.2 | 57.8±24.7 | 56.9±25.9 | .68 |
| Sodium, mEq/L | 138.7±4.6 | 139.0±4.3 | 138.1±5.1 | .03 |
| Echocardiogram, electrocardiographic data | ||||
| Left bundle branch block, % | 18.8 | 21.6 | 14.4 | <.05 |
| Right bundle branch block, % | 12.2 | 11.2 | 13.8 | .40 |
| LVH, % | 28.5 | 26.2 | 32.3 | .16 |
| LVEF, % | 52.5±14.8 | 49.8±15.4 | 56.9±12.8 | <.01 |
| LVEF≥50%, % | 64.3 | 56.2 | 77.4 | <.01 |
| Main cause of HF, % | ||||
| Hypertension | 45 | 39.5 | 54.4 | .001 |
| Ischemic heart disease | 29.5 | 36.9 | 17.4 | <.001 |
| Others | 25.5 | 23.6 | 28.2 | .7 |
| Treatment, % | ||||
| Diuretics | 90.5 | 93.8 | 85.1 | <.01 |
| ACE inhibitors or ARB | 82.7 | 86.2 | 76.9 | <.01 |
| Spironolactone | 28.3 | 30.6 | 24.6 | .16 |
| Digoxin | 26.6 | 24.4 | 30.3 | .15 |
| Statins | 43.1 | 50.9 | 30.3 | <.01 |
| Dicoumarin | 52.0 | 50.3 | 54.9 | .32 |
| ASA | 35.9 | 41.6 | 26.7 | <.01 |
ACE, angiotensin-converting enzyme; AMI, acute myocardial infarction; ARB, angiotensin receptor blocker; ASA, acetylsalicylic acid; BB, beta-blocker; BMI, body mass index; COPD, chronic obstructive pulmonary disease; DAP, diastolic arterial pressure; HF, heart failure; LVEF, left ventricular ejection fraction; LVH, left ventricular hypertrophy; MDRD, Modification of Diet in Renal Disease; NYHA, New York Heart Association; SAP, systolic arterial pressure
Unless otherwise indicated, values are expressed as no. (%) or mean±standard deviation.
At the time of discharge, 62.1% of patients were prescribed BB. With regard to comorbid conditions, BB were used more frequently in those with myocardial infarction and less frequently in those with chronic obstructive pulmonary disease. In patients who received BB, functional class was better, and diastolic arterial pressure and heart rate were higher. As to concomitant treatment, diuretics, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, acetylsalicylic acid, and statins were prescribed more often in patients treated with BB than in those without.
Although the LVEF was significantly lower in the BB group, most of the patients included (56%) had HF with preserved ejection fraction. Only 15.7% of our patients had LVEF lower than 35%.
Beta-blocker Prescription and Rate of Events During Follow-upThe BB prescription rates at 3 months (65.6%) and 1 year (67.9%) were slightly higher than at the time of discharge (62.1%), although the differences were not significant (P>.05).
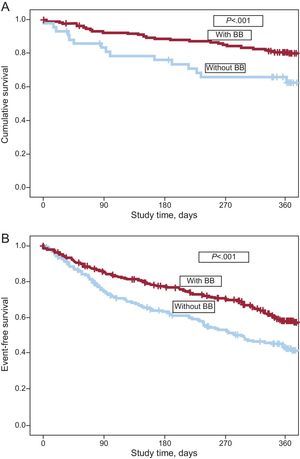
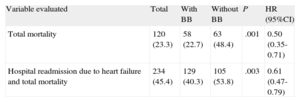
With regard to the mortality rate, there were 120 deaths during the year of follow-up (Figure 1), the majority (58.5%) due to HF. The remaining deaths were caused by other cardiovascular conditions (19%) and by noncardiovascular causes (22.5%). As can be seen in Table 2 and Figure 2, both the total mortality (Figure 2A) and the composite outcome, total mortality plus readmittance for HF (Figure 2B), were significantly lower in patients treated with BB than in those without (P<.001 and P<.003, respectively). On comparative analysis of BB prescription at discharge and at 1-year follow-up, there were no significant differences in percentages of prescription between the years 2008, 2009, 2010, and 2011 (59.9%, 64.3%, 62.2%, and 60.0%, respectively; P>.05).
Association between Beta-blocker Treatment and Mortality and Readmission for Heart Failure at 1 Year
| Variable evaluated | Total | With BB | Without BB | P | HR (95%CI) |
| Total mortality | 120 (23.3) | 58 (22.7) | 63 (48.4) | .001 | 0.50 (0.35-0.71) |
| Hospital readmission due to heart failure and total mortality | 234 (45.4) | 129 (40.3) | 105 (53.8) | .003 | 0.61 (0.47-0.79) |
95% CI, 95% confidence interval; BB, beta-blockers; HR, hazard ratio.
Values are expressed as no. (%).
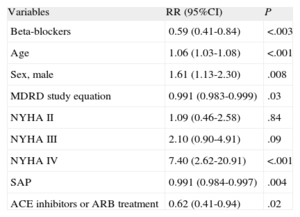
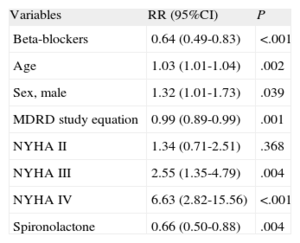
The results of multivariate analysis showed a significant association between BB administration and a reduction in total mortality (relative risk=0.59; 95% confidence interval, 0.41-0.84) and the composite variable, mortality and hospital readmittance (relative risk=0.64; 95% confidence interval, 0.49-0.83) (Tables 3 and 4). In addition to BB use, systolic arterial pressure, glomerular filtration rate, and the use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers were directly related to a reduction in mortality, whereas glomerular filtration and the use of spironolactone were associated with a reduction in the composite event.
Multivariate Analysis. Proportional Hazards Model: Mortality at 1 Year
| Variables | RR (95%CI) | P |
| Beta-blockers | 0.59 (0.41-0.84) | <.003 |
| Age | 1.06 (1.03-1.08) | <.001 |
| Sex, male | 1.61 (1.13-2.30) | .008 |
| MDRD study equation | 0.991 (0.983-0.999) | .03 |
| NYHA II | 1.09 (0.46-2.58) | .84 |
| NYHA III | 2.10 (0.90-4.91) | .09 |
| NYHA IV | 7.40 (2.62-20.91) | <.001 |
| SAP | 0.991 (0.984-0.997) | .004 |
| ACE inhibitors or ARB treatment | 0.62 (0.41-0.94) | .02 |
95%CI, 95% confidence interval; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; MDRD, Modification of Diet in Renal Disease; NYHA, New York Heart Association; RR, relative risk; SAP, systolic arterial pressure.
Variables included in the analysis: beta-blockers, age (years), sex (male), Modification of Diet in Renal Disease study equation, New York Heart Association functional class, systolic arterial pressure, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers treatment, hemoglobin, diabetes mellitus, acute myocardial infarction, peripheral arterial disease, stroke, atrial fibrillation, chronic obstructive lung disease, spironolactone, loop diuretics, digoxin, and left ventricular ejection fraction.
Multivariate Analysis. Proportional Hazards Models: Mortality or Readmission for Heart Failure at 1 Year
| Variables | RR (95%CI) | P |
| Beta-blockers | 0.64 (0.49-0.83) | <.001 |
| Age | 1.03 (1.01-1.04) | .002 |
| Sex, male | 1.32 (1.01-1.73) | .039 |
| MDRD study equation | 0.99 (0.89-0.99) | .001 |
| NYHA II | 1.34 (0.71-2.51) | .368 |
| NYHA III | 2.55 (1.35-4.79) | .004 |
| NYHA IV | 6.63 (2.82-15.56) | <.001 |
| Spironolactone | 0.66 (0.50-0.88) | .004 |
95%CI, 95% confidence interval; MDRD, Modification of Diet in Renal Disease; NYHA, New York Heart Association; RR, relative risk.
Variables included in the analysis: beta blockers, age (years), sex (male), Modification of Diet in Renal Disease study equation, New York Heart Association functional class, systolic arterial pressure, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers treatment, hemoglobin, diabetes mellitus, acute myocardial infarction, peripheral arterial disease, stroke, atrial fibrillation, chronic obstructive lung disease, spironolactone, loop diuretics, digoxin, and left ventricular ejection fraction.
In contrast, age, male sex, and functional class were predictive of both clinical events (Tables 3 and 4). We should mention that there was no association with other variables, such as LVEF, diabetes mellitus, acute myocardial infarction, or stroke.
DISCUSSIONThe results of our study show that 62% of patients hospitalized for HF in internal medicine departments, mainly elderly persons, receive BB treatment, regardless of whether they have decreased LVEF. It should be noted that this percentage was maintained at 3 and 12 months of follow-up, indicating that BB treatment is well tolerated by the elderly HF population. Although BB are a basic therapeutic measure for HF, the use of these drugs in persons of advanced age is limited, with prescription rates clearly lower than 50% in most observational studies.18–20 The limited prescription of BB in this population has been attributed to various reasons: the fact that elderly patients are rarely included in most clinical trials; the absence of consistent evidence regarding optimal treatment for HF with preserved ejection fraction, the predominant type in this age group; the comorbid conditions in these patients; and frequent use of multiple medications, with a potential risk of adverse effects and decreased tolerance.21,22 Nonetheless, recent clinical practice studies have documented an increase in BB use in HF patients, with values similar to those in the RICA registry.23 Furthermore, results from clinical trials and prospective observational studies have confirmed that elderly patients have excellent tolerance of BB.24,25 In the BETANIC study, conducted by the SEMI HF group in a population with a mean age of 79 years, we found that 80% of BB-treated patients remained on treatment at 6 months of follow-up.26 Furthermore, the CARACTER-BETA study documented a BB prescription rate of 64% in hospitalized patients and ambulatory patients seen in internal medicine services.27 These findings demonstrate a considerable increase in BB use relative to the 2002 rate of 10%.6 Of note, the use of BB in elderly patients is justified not only for the HF, in itself, but also for the elevated prevalence of atrial fibrillation (more than 51% in our cohort). Furthermore, although it was not the main objective of the study, we observed a significant decrease in clinical events (total mortality and total mortality plus hospital readmissions for HF) at one year of follow-up in patients treated with BB at hospital discharge. It should be mentioned that the benefits of BB with regard to mortality were independent of other factors, such as LVEF, acute myocardial infarction, stroke, or diabetes mellitus. These findings are especially important in cases of HF with preserved ejection fraction, in whom there is little existing evidence regarding the utility of BB use.7,8,11
Our study sample is representative of patients attended in internal medicine departments, as is evidenced by their advanced age and multiple comorbidities, similar to the characteristics of the population included in the CARACTER-BETA study, also attended by internists. Therefore, the results cannot be extrapolated to patients in cardiology services, who are usually younger and have fewer comorbidities.27
Strengths and LimitationsPossibly the main strength of the RICA registry is that it is representative of the elderly HF population, who are usually seen in hospital internal medicine services: advanced age, marked comorbidity, and predominance of women with HF and preserved ejection fraction.28 However, our study also has some limitations. Because sequential analysis of the data from each patient in the various phases of follow-up was not performed, we cannot precisely know how many patients underwent a change in BB treatment (discontinuation or start after discharge). Nor was it the aim of the study to determine the reasons why BB treatment was not prescribed or was discontinued, or what doses were used. However, the clinical differences between patients treated or not with BB were those expected: higher acute myocardial infarction rate, functional class III-IV, lower rate of chronic obstructive pulmonary disease, and lower LVEF in treated patients. In any case, the results clearly demonstrate more frequent use of this treatment than in previous observational evaluations. There were relatively few cases with missing information during follow-up (21 cases), with no differences between those taking BB or not. Therefore, we do not believe that this factor would cause a relevant change in the data. Finally, the results regarding the influence of BB use on the prognosis should be confirmed in a randomized controlled study.
CONCLUSIONSThe data from the RICA registry show that BB use in elderly patients with HF is more prevalent now than in previous studies, regardless of the patient's LVEF, and indicate that this treatment is associated with a benefit in reducing clinical events. Therefore, there is no reason for undue concern about the use of these drugs in the elderly population. Programs that further enhance the implementation of this treatment at recommended doses in clinical practice should be encouraged, particularly in relation to elderly patients.
CONFLICTS OF INTERESTNone declared.
We are very grateful to all the investigators who participate in the RICA registry. Our thanks to the coordinating center of RICA, S & H Medical Science Service, for their work in monitoring, and their logistic and administrative support.
L. Anarte, O. Aramburu, J.C. Arévalo, J.L. Arias, A. Armengou, F. Bas-Sanchis, P. Bettencourt, F.J. Carrasco, M. Carrera, J. Casado, L.M. Ceresuela, J.M. Cerqueiro, D. Chivite, A. Conde, M.F. Dávila, J. Díez-Manglano, F. Epelde, F. Formiga, J. Franco, A. González-Franco, J. Grau-Amorós, R. Oropesa, C. Pérez-Bocanegra, J.I. Pérez-Calvo, M.A. Quesada, P. Llacer, L. Manzano, M. Montero, A. Muela, I. Murado, J. Recio, N. Ribas, B. Roca, F. Ruiz-Laiglesia, M.P. Salamanca, J.C. Trullàs, M. Sánchez-Marteles, C. Sánchez, J.L. Santiago, J.A. Satué, A. Serrado, and A. Urrutia.