To analyze the clinical status of patients with “uncorrected” scimitar syndrome in a multicenter Italian study.
MethodsThe natural history of scimitar syndrome was analyzed in 44 affected individuals (from 9 Italian centers).
ResultsThe median age at diagnosis was 1.05 years (range, 1 day-41 years). Thirty-three patients (75%) had an isolated form; 11 patients (25%) had associated congenital heart diseases. Twenty-two patients (50%) were symptomatic at diagnosis, including respiratory symptoms (n=20) and congestive heart failure (n=6). Patients with associated congenital heart defects had a higher prevalence of congestive heart failure (4 of 11 [36.4%] vs 2 of 33 [6.1%]; P=.027), pulmonary arterial hypertension (7 of 11 [63.6%] vs 2 of 33 [6.1%]; P=.027) than patients with isolated forms. Ten patients (22.7%) underwent correction of associated cardiac defects, leaving the anomalous pulmonary venous drainage intact. The median length of follow-up after diagnosis was 6.4 years (range, 0.2-27.5 years). Two patients died, both with associated cardiac defects and severe pulmonary arterial hypertension. Of 42 survivors, 39 (92.8%) were asymptomatic at the last follow-up visit; 3 patients still complained respiratory symptoms. There was no difference between isolated and associated forms of the disease.
ConclusionsIn most patients, scimitar syndrome presented as an isolated lesion with a benign outcome. Nonetheless, when associated with other cardiac defects and pulmonary arterial hypertension, there was an increased risk of congestive heart failure and mortality. Correction of associated cardiac defects (transforming “associated” into “isolated” forms), together with the therapeutic occlusion of anomalous arterial supply to the lung, led to a benign outcome comparable to that in primarily isolated forms.
Keywords
Scimitar syndrome is a rare association of cardiopulmonary anomalies and represents only 3% to 6% of all forms of partial anomalous pulmonary venous connections.1–4 Both the right lung and the right pulmonary artery are frequently hypoplastic and the lung receives its blood supply from systemic collaterals mainly arising from the thoracic or the abdominal aorta.5–8 An associated atrial septal defect is found in approximately 60% to 70% of patients with scimitar syndrome, and other congenital heart diseases (CHDs) are associated in 19% to 31%.
The decision-making process for surgical correction is often challenging, and there is still no consensus on the correct indications and the ideal timing of repair, especially in asymptomatic patients who are frequently diagnosed incidentally.9–12
The objective of this study was to analyze the clinical status of patients with scimitar syndrome who did not undergo surgical repair of the anomalous venous drainage and who underwent follow-up of the natural history of their disease within an Italian multicenter study.
METHODSA review of the medical records and computerized hospital data was approved by the Ethical Committee of the University Hospital of Padua, and the procedures followed were in accordance with the institutional guidelines for retrospective record review and protection of patient confidentiality. The data reviewed were related to the in-hospital clinical course and to the follow-up status of patients with scimitar syndrome who did not undergo surgical correction of the anomalous pulmonary venous drainage (“scimitar drainage”) and who underwent follow-up of the natural history of the syndrome from January 1997. Data collection was carried out in 9 Italian pediatric cardiology centers within the Italian Society of Pediatric Cardiology.
In this study, the patients were divided in 2 groups: group 1 included patients with isolated scimitar syndrome (without hemodynamically significant associated CHDs, thus including patients with a patent foramen ovale) who did not require surgical treatment; group 2 included patients with associated CHDs who required treatment of associated congenital heart defects.
The variables analyzed included patient age at diagnosis, the presence of symptoms at the time of diagnosis, including both congestive heart failure (CHF) and respiratory symptoms (due to recurrent upper respiratory tract infections, pneumonia, and hemoptysis), the presence of pulmonary arterial hypertension (PAH) (defined as a mean pulmonary artery pressure greater than 25mmHg at rest), and the presence of moderate-severe right ventricular dilation. We also considered the impact of hemodynamic procedures (ie, interventional coil embolization of aortopulmonary collaterals or other interventional maneuvers in associated CHDs including percutaneous occlusion of patent ductus arteriosus) and the impact of surgical procedures on associated CHD (leaving scimitar vein drainage intact) on patient outcome.
The primary outcome was the patients’ clinical status at the end of follow-up (defined as the presence of symptoms).
The association between dichotomous variables was verified by Fisher's exact test. Quantitative variables were compared by using the Wilcoxon signed rank test. The significance level was set at 0.05. Data were analyzed using SAS Stat 9.2® (SAS Institute Inc.; North Carolina, United States).
RESULTSForty-four patients were included from 9 Italian centers (median of 3.5 patients per center [range, 1-20 patients]), There were 25 women (56.8%) and 19 men (43.2%). In all patients, diagnosis was established by chest X-ray and echocardiography. Additional instrumental examinations included cardiac catheterization in 31 patients (70.4%), computed tomography in 16 patients (36.3%) and magnetic resonance angiography in 11 patients (25%).
Thirty-three patients (75%) presented with an isolated form of scimitar syndrome. The remaining 11 patients (25%) presented with other associated CHD including an atrial septal communication, secundum type (n=4), a patent ductus arteriosus (n=6), a ventricular septal defect (n=4), an aortic isthmic coarctation (n=2), and a mixed anomalous pulmonary venous connection (including “scimitar vein drainage” and a partial anomalous pulmonary venous drainage of the left superior pulmonary vein into the innominate vein through a vertical collector vein) (n=1). Five patients had 2 or more associated CHDs (excluding a patent foramen ovale).
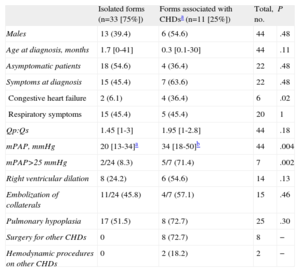
The median age of the patients at diagnosis was 1.05 years (range, 1 day-41 years). Prenatal two-dimensional-echo diagnosis was possible in 2 patients. Twenty-two patients (50%) were symptomatic at the time of diagnosis; symptoms included respiratory symptoms (n=20) (caused by recurrent respiratory infections in 20 patients and by recurrent hemoptysis in 1 patient) and CHF (n=6). Four patients had both CHF and respiratory symptoms. Two of the 33 patients with the isolated form of scimitar syndrome had CHF at diagnosis (2 of 33 [6.1%] vs 4 of 11 [36.4%] patients with associated CHDs; P=.027) (Table 1). No correlation was found between patient age and the presence of significant right lung hypoplasia and the presence of symptoms at diagnosis.
Demographics, Clinical Status at Diagnosis and Hemodynamic Parameters According to the Different Forms of Scimitar Syndrome (n=44 Patients)
| Isolated forms (n=33 [75%]) | Forms associated with CHDsa (n=11 [25%]) | Total, no. | P | |
| Males | 13 (39.4) | 6 (54.6) | 44 | .48 |
| Age at diagnosis, months | 1.7 [0-41] | 0.3 [0.1-30] | 44 | .11 |
| Asymptomatic patients | 18 (54.6) | 4 (36.4) | 22 | .48 |
| Symptoms at diagnosis | 15 (45.4) | 7 (63.6) | 22 | .48 |
| Congestive heart failure | 2 (6.1) | 4 (36.4) | 6 | .02 |
| Respiratory symptoms | 15 (45.4) | 5 (45.4) | 20 | 1 |
| Qp:Qs | 1.45 [1-3] | 1.95 [1-2.8] | 44 | .18 |
| mPAP, mmHg | 20 [13-34]a | 34 [18-50]b | 44 | .004 |
| mPAP>25 mmHg | 2/24 (8.3) | 5/7 (71.4) | 7 | .002 |
| Right ventricular dilation | 8 (24.2) | 6 (54.6) | 14 | .13 |
| Embolization of collaterals | 11/24 (45.8) | 4/7 (57.1) | 15 | .46 |
| Pulmonary hypoplasia | 17 (51.5) | 8 (72.7) | 25 | .30 |
| Surgery for other CHDs | 0 | 8 (72.7) | 8 | − |
| Hemodynamic procedures on other CHDs | 0 | 2 (18.2) | 2 | − |
CHD, congenital heart disease; mPAP, median pulmonary arterial pressurea.
Data are expressed as no. (%) or median [range].
Significant right lung hypoplasia was found in 25 patients (56.8%) and there was no difference between groups in the prevalence of significant lung hypoplasia (17 of 33 [51.5%] in group 1 vs 8 of 11 [72.7%] in group 2; P=.301). One patient presented with a horseshoe lung (Figure).
Moderate-to-severe right ventricular chamber dilatation was assessed in 14 patients (31.8%); patients with associated CHD had a higher prevalence of moderate-to-severe right ventricle dilatation (6 of 11 [54.5%] vs 8 of 33 [24.2%] in patients with isolated forms; P=.132).
At cardiac angiography, a systemic arterial supply to the right lung was demonstrated in 24 of 31 patients (77.4%); of these, 15 were treated by coil embolization. The median mean pulmonary artery pressure was 20mmHg (range, 13-50mmHg) (Table 1). Seven patients (7 of 31 [22.5%]) presented with PAH (demonstrated by angiography); patients with associated CHD had a higher prevalence of PAH (2 of 24 [8.3%] in group 1 and 5 of 7 [71.4%] in group 2; P<.0001).
All patients with associated CHDs underwent repair of their cardiac malformations without correction of the anomalous pulmonary venous connection (scimitar collector).
Nine patients underwent surgical treatment including: a) atrial septal defect secundum type closure (n=4); b) ventricular defect closure (n=4); c) patent ductus arteriosus ligation (n=6); d) isthmic coarctation repair (n=2), and e) correction of the left anomalous pulmonary venous drainage in the patient with a mixed anomalous pulmonary venous connection (n=1). In 2 of these patients the diagnosis of scimitar syndrome was reached incidentally, a few years after the closure of an atrial septal communication. In the remaining 7 patients, all with significant right lung hypoplasia, the anomalous pulmonary venous drainage was deemed not hemodynamically significant at the time of diagnosis and was not treated.
The remaining 2 patients with associated CHDs underwent percutaneous patent ductus arteriosus occlusion during angiographic evaluation.
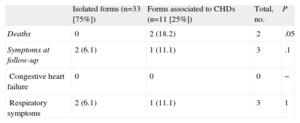
Follow-upThe median follow-up was 6.4 years (range, 0.2-27.5 years). None of the patients underwent correction of scimitar vein drainage. Two patients (4.5%), both with associated CHDs at diagnosis, died: the first died at the age of 14 months from CHF and severe untreatable pulmonary hypertension and the second died at the age of 5 months from CHF, pulmonary hypertension and acute renal failure after surgical correction of a left anomalous pulmonary venous drainage.
Thirty-nine patients (39 of 42 survivors [92.8%]) were asymptomatic at the last follow-up visit (31 patients with isolated scimitar syndrome [93.9%] and 8 patients with the associated form [88.8%]). Three patients still had respiratory symptoms (age at follow-up was 2.7, 6.0 and 47.2 years) (Table 2). Twenty-two patients have never complained of symptoms (22 of 42 survivors [52.3%]), whereas 17 patients (17 of 42 [40.7%]) had improved clinical status, mainly presenting with respiratory symptoms at diagnosis (16 of 17 patients). The clinical status of 4 patients with CHF at diagnosis also improved: a) following the correction of associated CHDs plus embolization of collaterals in 2 patients with associated CHDs, and b) following embolization of collaterals in 2 patients with isolated forms.
Outcomes and Clinical Status at Follow-up According to the Different Forms of Scimitar Syndrome (n=44 Patients)
| Isolated forms (n=33 [75%]) | Forms associated to CHDs (n=11 [25%]) | Total, no. | P | |
| Deaths | 0 | 2 (18.2) | 2 | .05 |
| Symptoms at follow-up | 2 (6.1) | 1 (11.1) | 3 | .1 |
| Congestive heart failure | 0 | 0 | 0 | − |
| Respiratory symptoms | 2 (6.1) | 1 (11.1) | 3 | 1 |
CHD, congenital heart disease.
Data are expressed as no. (%).
Scimitar syndrome is a rare CHD characterized by the association of various cardiothoracic malformations and a wide clinical spectrum of presentation.
It is widely accepted that the infantile form, due to its severity, usually requires prompt intervention to relieve clinical symptoms, especially when associated with complex cardiovascular anomalies and PAH.3,12–16
However, many of these patients are incidentally diagnosed during infancy and adulthood and usually remain asymptomatic or mildly symptomatic for many years, leading a normal life without surgical repair.3,17–19
Surgical correction of the anomalous pulmonary venous return is usually accomplished in symptomatic patients or in patients with an increased pulmonary blood flow and signs of right heart chamber dilation and consists of redirection of the anomalous pulmonary venous connection into the left atrium or the removal of part of or the whole of the right lung in patients with severe clinical features.3,9,12 When planning the most appropriate surgical approach, complete preoperative knowledge of the course of anomalous venous return and systemic collateral arteries is useful. However, surgery is not free of complications and, based on the suboptimal results of surgical repair from previous reports,3,4,20 affected individuals require continuous clinical follow-up to assess their clinical status and the long-term patency of the scimitar vein.
With this concept in mind, based on multi-institutional data collection, we evaluated the clinical outcome of patients with scimitar syndrome who underwent follow-up of the natural history of the anomaly (without correction of scimitar vein drainage) with particular emphasis on patients with isolated forms: in our opinion, these latter patients represent a challenging subset of patients when choosing the ideal treatment option.
According to our results, the majority of patients (75%) had an isolated form of scimitar syndrome, which was diagnosed incidentally, and most were asymptomatic. In contrast, patients with associated CHDs had a greater association with preoperative CHF and more frequently had associated PAH. Overall, almost half of the patients had respiratory symptoms at diagnosis, with no difference between patients with isolated forms and those with associated CHDs.
At the last follow-up visit, at a median of 6.4 years after the initial diagnosis, we found a significant decrease in the prevalence of respiratory symptoms, which mainly suggested a decreasing prevalence with age (20 of 44 [45.4%] at diagnosis vs 3 of 42 [7.1%] at follow-up). The surgical treatment of associated CHDs (leaving the anomalous venous connection intact and transforming an associated form to an isolated form of scimitar syndrome) proved safe and effective, with no significant difference in symptomatic patients between groups at the last follow-up visit. Notably, none of the patients in either group had signs of CHF at the final follow-up visit.
In agreement with previous reports, the presence of PAH is the most important prognostic factor in patient outcome and may be related to the presence of coexisting CHDs, to high resistances in the pulmonary vascular bed (where the pulmonary circulation fails to adapt normally after birth) and to a large shunt between abnormal arteries arising from the abdominal aorta and supplying the lower part of the right lung.4,21–24 For this reason, therapeutic occlusion of any anomalous arterial supply to the lung, when demonstrated, should be accomplished either by preoperative coil embolization or at the time of surgical repair, thus reducing the amount of blood flow to the lungs and intracardiac shunts.25,26
LimitationsThe design of this study has some limitations. This was a retrospective study that included a medium-term follow-up evaluation of patients of all ages with scimitar syndrome. Cardiac catheterization was performed in only a few patients in our cohort; therefore, some important data such as the Qp:Qs and the median pulmonary artery pressure were not available in all patients. In addition, because data were collected in 9 centers, there may be interinstitutional and intrainstitutional variability in the evaluation of risk factors.
Nonetheless, we have collected a complete series of data on a relatively large series of patients who did not undergo surgical correction of their anomalous right pulmonary venous connection (scimitar drainage) and who underwent follow-up of the natural history of their anomaly in the context of a rare congenital heart malformation.
CONCLUSIONSScimitar syndrome presents as an isolated lesion in the majority of patients who are usually asymptomatic. The correction of associated CHDs (transforming “associated” into “isolated” forms), together with therapeutic occlusion of anomalous arterial supply to the lung, may lead, in selected patients, to a benign outcome that is maintained over time, as in the primarily isolated forms. Nonetheless, when scimitar syndrome is associated with other CHDs and PAH there is an increased risk of CHF and mortality.
Continuous clinical and noninvasive follow-up is indicated in these patients to determine any clinical or physiological variations and to plan the most appropriate treatment.27,28
Because scimitar syndrome is almost always associated with right lung hypoplasia and the scimitar vein often carries a small amount of blood flow, surgical correction of the anomalous pulmonary venous return should be considered only when the scimitar drainage has been proven to cause a considerable amount of pulmonary overload. An angiographic study is recommended if there is persistence or worsening of clinical symptoms or if there is elevated pressure in the pulmonary arterial tree (by indirect measurement through two-dimensional echocardiography).
CONFLICTS OF INTERESTNone declared.