Keywords
THE SCOPE OF THE PROBLEM
Cardiovascular diseases (CVD), of which coronary heart disease (CHD) is the most common, are the major causes of death in middle-aged and older patients in most developed countries and in many developing countries.1-3. Cardiovascular diseases result in substantial disability worldwide and contribute in large part to the escalating costs of healthcare, especially with an increasing ageing population.4 Cardiovascular diseases place an immense burden on both patients and community and are predicted to be the leading cause of death and disability-adjusted life years by 2020. This is largely because of an increasing of CVD in developing countries.5
According to a recent publication of the World Health Organisation (WHO), cardiovascular diseases accounted for 30% of an estimated 58 million deaths globally from all causes in 2005.1 CVD is a leading cause of global mortality, accounting for nearly 17.5 million deaths every year. Nearly 80% of this global mortality and disease burden occurs in developing countries. In 2001, cardiovascular disease was the leading cause of death in 5 of the 6 WHO regions. Between 2006 and 2015, deaths due to noncommunicable diseases (half of which will be due to cardiovascular disease) are expected to increase by 17%, while mortality from infectious diseases, nutritional deficiencies, and maternal and perinatal conditions combined is projected to decline by 3%.6,7. Almost half of the disease burden in low- and middle-income countries is already due to noncommunicable diseases. The projected increase in CVD mortality can be related to an increase in life expectancy due to public health initiatives reducing infectious diseases, nutritional deficiencies, and perinatal complications, and to improved economic conditions. Adverse lifestyle changes associated with industrialisation and higher income in some population groups, and the longer life expectancy increase the degree and duration of exposure to cardiovascular risk factors. The increased tobacco use and unhealthier diet with high fat and calorie intake which are now present in the economically developed countries are becoming established in the developing countries. Tobacco consumption is responsible for about 5 million deaths in 2003, mostly in poor countries and poor populations and the number of deaths will double in 20 years unless effective interventions are urgently implemented. A significant proportion of cardiovascular morbidity and mortality could be prevented through population based strategies, and by making cost-effective interventions accessible and affordable, both for people with established disease and for those at high risk of developing cardiovascular disease.8,9
GLOBAL PREVENTIVE POLICIES
The rising burden of noncommunicable diseases was addressed by the 53rd World Health Assembly in May 2000 which adopted the WHO Global Strategy for the Prevention and Control of Noncommunicable Diseases.10 The noncommunicable diseases were placed on the global public health agenda. As described in the Global Strategy for the Prevention and Control of Noncommunicable Diseases, one of the major tasks for WHO and its Member States is to scale up cost-effective, integrated approaches for prevention of CVD. Although CVD already places a significant economic burden on low- and middle-income countries, the resources available for its management in these countries are limited because of competing health priorities.11 It is, however, essential to recognize that the transition to lower levels of infectious diseases and higher levels of noncommunicable diseases is already under way; failure to act now will result in large increase in CVD, placing serious pressures on the national economies.12-14 In this context, it is imperative to target the limited resources on those who are most likely to benefit.
In the global effort to reduce morbidity and mortality from CVD, the World Heart and Stroke Forum (WHSF) Guidelines Task Force of the World Heart Federation(WHF) recommends that every country develop a policy on CVD prevention.15 National policy should be developed by systematic and ongoing dialogue among governmental, public health, and health professional groups. National policy should set priorities for public health and clinical interventions appropriate to the country and should also be the foundation for the development of national guidelines on CVD prevention.
While the causes of CVD are common to all parts of the world, the approaches to cardiovascular prevention at a societal or individual level will differ between countries for cultural, social, medical, and economic reasons. Although national guidelines will embrace the principles of CVD prevention recommended in this report, they may differ in terms of the organisation of preventive cardiology, risk factor treatment targets, and the use of cardioprotective medications. The recommendations in this report focus on clinical management of patients with established CVD and those at high risk; however, it is essential that each country include a societal approach to CVD prevention.15 As stated in the WHO publication Integrated Management of Cardiovascular Risk, "Epidemiological theory indicates that, compared with intensive individual treatment of high-risk patients, small improvements in the overall distribution of risk in a population will yield larger gains in disease reduction, when the underlying conditions that confer risk are widespread in the population."16 Each country should seek to implement national clinical guidelines directed toward high-risk individuals and give equal importance to developing low-risk population strategies.
The globalisation of tobacco and obesity epidemics was recognised by the WHO which has strengthened its efforts to promote population-wide primary prevention of noncommunicable diseases, through the Framework Convention on Tobacco Control17 and the Global Strategy for Diet, Physical Activity, and Health.18 These activities target common risk factors that are shared by CVD, cancer, diabetes, and chronic respiratory disease, and their implementation is crucial for controlling the increased burden of noncommunicable diseases.
These strategies should make it easier for healthy people to remain healthy, and for those with established CVD or at high cardiovascular risk to change their lifestyle. However, population-wide public health approaches alone will not have an immediate substantial impact on cardiovascular morbidity and mortality, and will have only a modest absolute impact on the disease burden.5,8 By themselves they cannot help the millions of individuals at high risk of developing CVD or with an established CVD. A combination of population-wide strategies and strategies targeted at high risk individuals is needed to reduce the burden of cardiovascular disease. The extent to which one strategy should be emphasized over the other depends on achievable effectiveness but also on cost-effectiveness and availability of resources.4-7
STRATEGY PLANNING
The 1992 Report of the World Health Organisation Expert Committee on Prevention of Coronary Heart Disease19 considered that a comprehensive action for CVD prevention has to include 3 components:
1. "Population" strategy: for altering, in the entire population, the lifestyle and environmental factors, and their social and economic determinants, that are the underlying causes of the mass occurrence of CVD.
2. "High-risk" strategy: identification of high risk individuals, and action to reduce their risk factor levels.
3. Secondary prevention: prevention of recurrent cardiovascular events and progression of the disease in patients with clinically established coronary or other atherosclerotic disease.
The population strategy is the essential way to reduce the incidence and the burden of cardiovascular diseases when the risk is widely distributed across society as a whole. The aim of this strategy is to reduce cardiovascular risk in the entire population regardless of each individual's level of risk and potential benefits. The population strategy aims at shifting the distribution of risk factors towards more favourable levels through actions directed to change the environment and lifestyle of individuals, without the need to medically examine them, in order to reduce the incidence of disease by preventing or delaying the occurrence of acute cardiovascular events and the progression of chronic disease.20 It aims to reduce the risk factors at population level through lifestyle and environmental changes affecting the whole population. In its traditional "public health" form population strategy has involved mass environmental control methods; in its modern form it is attempting to modify some of society's norms of behaviour. This type of strategy is mostly achieved by establishing planned policies and community interventions. Without a well resourced national population strategy dealing with the major cardiovascular risk factors, they will remain a major cause of disease and premature death, regardless of the fact that individual lives might be saved.
The population strategy has several disadvantages. First, to prevent one single cardiovascular event, it will be necessary to intervene upon many subjects with no apparent benefit to them. This leads to the prevention paradox: "a preventive measure which brings much benefit to the population offers little to each participating individual."20 Second, the number of individuals needed to treat to prevent one event will vary in different populations or population subgroups (for example in women) depending on their underlying prevalence of cardiovascular risk factors. This problem can be resolved by estimating the absolute total multifactorial risk to trigger intervention, which helps to avoid over-treatment of low risk young women and under treatment of high risk middle aged men.
The high-risk primary prevention strategy deals with healthy persons with high absolute risks of future disease and the secondary prevention strategy is focussed on patients with established cardiovascular or other atherosclerotic disease. However, since cardiovascular risk is a continuum, with many asymptomatic high risk people having investigative evidence of atherosclerosis, the terms "primary" and "secondary" prevention are artificial.2 The high-risk strategy has some important advantages. First, it leads to intervention which is appropriate to individual and is focused on people likely to benefit the most from it. Second, the "high-risk" strategy offers a more cost-effective use of resources. This strategy aims to diminish the total cardiovascular risk of individuals belonging to the upper part of the risk distribution.
In constructing preventive policies, choices need to be made between different strategies.7 For instance, will preventing small risks in large populations avoid more adverse events than avoiding large risks in a smaller number of high-risk individuals? What priority should be given to cost-effective interventions for primary rather than secondary prevention, such as lowering blood pressure by reducing dietary salt intake compared with treatment of people with high blood pressure?
In practice population and high-risk strategies are usually combined so as to complement each other.21 The difference between the groups will be reflected in the priorities for intervention and the intensity of treatment.
Focusing on high-risk individuals can reduce costs at the population level because an intervention is provided to fewer people, but on the other hand it might also increase the costs of identifying the group of people most likely to benefit. Focusing on people who are more likely to benefit has a significant impact on the health of a nation only when there are large numbers of them. For example, lowering cholesterol with drugs is effective in reducing overall mortality in a group of people at high risk of dying of cardiovascular disease. However, only a small percentage of the population is at high risk of death from heart disease at any given time, and only some of them can be identified purely on the basis of their cholesterol levels. The evidence suggests that the group most likely to benefit from cholesterol reduction consists of individuals with combinations of risk factors, such as being male, smoker, obese and not physically active, and having raised blood pressure, and elevated cholesterol. Designing interventions for people with a combination of those risk factors is proven to be more effective than treating people only on the basis of their levels of blood pressure or cholesterol. This form of targeted approach is called the "absolute risk approach."
In general, population-wide interventions have the greatest potential for prevention. For instance, in reducing risks from blood pressure and cholesterol, shifting the mean of whole populations will be more cost-effective in avoiding future heart attacks and strokes than screening programmes that aim to identify and treat all those people with elevated blood pressure or raised cholesterol levels. The term "screening" refers to organized public health action targeting to examine the population at risk to diagnose earlier stages of disease under the assumption that earlier treatment will be more beneficial than treatment at later stages of disease development. There is no evidence that mass screening for detection of early stages of CHD or stroke is cost-effective. The screening for lifestyle and other risk factors associated with future disease should focus in those at high risk. But to identify those at high risk, it is necessary to examine periodically everyone in the population, which could be unfeasible for any health system. So, the population strategy has the potential to improve population health to a much greater extent than a high-risk approach, while at the same time reducing the costs of identifying high-risk people. On the other hand, the costs of providing an intervention to the entire population would, in this case, be higher than providing it only to people at high risk. Which approach is the most cost-effective in any setting will depend on the prevalence of high-risk people in the population and the costs of identifying them. Both strategies are necessary and complement each other and the balance between them will depend on the absolute mean level of risk and its distribution in each specific population. Often both approaches are used and successfully combined in one strategy.
Risk prevention will be successful if the leaders from the ministries of health and the public health communities are determined to take the appropriate political decision and plan the strategy for CVD prevention.7 Important factors which determine whether adopted policies include public perceptions of the risks and benefits, perceived levels of scientific uncertainty, and how widely the risks and health outcomes are distributed. The success of policies can be influenced by the special interest groups and the media, and more effective communication about the prevention strategies by the governments and the scientific community.
The national circumstances are very important for choosing the strategy for CVD prevention. In many middle and low income countries there is a lack of scientific expertise and medical equipment making local cardiovascular risk assessment very difficult. In some developing countries, cardiovascular diseases may also be considered as a low priority for special political action by the government. Therefore, public awareness and knowledge about cardiovascular diseases need to be enhanced through effective communication by the special interest groups and the mass media.
The ministries of health have to take the leadership for political action for prevention of cardiovascular disease at national level. However the collective actions at regional and international levels are also required. This is where the World Health Organization can play an effective advisory and coordinating role.
Many different combined interventions to reduce the risk of CVD are possible—for example, in 2002 WHO recommended the integrated management of cardiovascular diseases by focusing on blood pressure, smoking cessation, and diabetes.22 It this document, the combination of population interventions and management of total multifactorial risk in high risk people is recommended as the most effective approach for prevention. The population-wide interventions involve using the mass media for increasing risk factors knowledge and legislation for banning smoking and salt reduction. The absolute risk approach should be an alternative to focusing on cholesterol or blood pressure levels separately. It should be used to evaluate individual's risk of a cardiovascular event in the next 10 years. All people with an estimated multifactorial risk of a cardiovascular event over the next decade that exceeds a given threshold should be provided with lifestyle education and their multiple risk factors should be managed to target. The calculation of total risk of a cardiovascular event usually is based on age, sex, body mass index, serum total cholesterol, systolic blood pressure levels, and smoking status. In countries with poorer economic resources, lower cost and more practical implementation strategies could result in risk assessment solely on the basis of age, sex, smoking status, and body mass index.1
STRATEGIES AT EUROPEAN AND WORLDWIDE LEVEL
The International Heart Health Conferences issued declarations on prevention of CVD in 1992 (Victoria Declaration),23 in 1996 (Catalonia Declaration),24 in 1998 (Singapore Declaration),25 and in 2001 (Osaka Declaration).26
The Singapore Declaration particularly describes the principles underlying the strategies to prevent CVD.25 The principles are divided into those relevant to the structure of cardiovascular preventive programs and those appropriate to the political will to proceed to action. Preventive efforts have been logically extended by different international organizations with more specific agendas for longer periods of time. The idea is that the clinicians, researchers, and others health professionals have to accept personal responsibility and to assume a leadership role in the field of CVD prevention. In the section on physical and organizational infrastructure of prevention, the Singapore Declaration specifies the importance of nongovernmental organizations and professional health organizations such as the WHF. The national societies of cardiology and related professional organisations should assume leadership of continental and national programs to prevent further increases in the occurrence of CVD. Societies of cardiology have the professional authority to not only ask government to allocate resources for care of patients with CVD but also to incorporate prevention of CVD into legislation whenever relevant.15
The Osaka Declaration recommended the following health, economic and political actions aroused from the fourth International Heart Health Conference in 200126:
- Increase awareness of governments that the health agenda is not just an agenda of health departments
- Let scientists and health professionals contribute to the marketing of the heart health agenda
- Let schools for health professionals provide training in methods for community organizing, social marketing, and advocacy
- Let departments of health, non-governmental organisations (NGOs), and professional organizations develop plans to make the case for heart health resources at the political level
- Let the WHO continue to strengthen the capacity for heart health promotion in all WHO regions and member states
The first International Principles for National and Regional Guidelines on CVD Prevention were published by the WHF in 2004. The World Heart and Stroke Forum of the WHF recommends 10 strategic principles as a template for the development of national clinical guidelines15:
- Governments, national societies, and foundations should collaborate to develop clinical and public health guidelines for CVD prevention that target risk factors
- Evidence-based guidelines should incorporate professional judgment on the translation of such evidence into effective and efficient care addressing all areas of CVD risk
- The assessment of total CVD risk should be based on epidemiological risk factor data appropriate to the population to which it is applied
- Policy recommendations and guidelines should emphasize a total risk approach for CVD prevention
- The intensity of interventions should be a function of the total risk of CVD, with lower treatment thresholds for higher-risk patients
- National cardiovascular societies/foundations should promote routine prospective collection of validated national vital statistics on the causes and outcomes of CVD for use in the development of national policies
- National professional societies should inform policymakers of risk factor targets and drug therapies for prevention of CVD that are culturally and financially appropriate to their nation and ask the government to incorporate prevention of CVD into legislation whenever relevant
- National professional societies/foundations should facilitate CVD prevention through education and training programs for health professionals
- National professional societies should assess the achievement of lifestyle, risk factor, and therapeutic targets defined in the national guidelines
- Health professionals should include prevention of CVD as an integral part of their daily clinical practice.
Although the focus of these recommendations is clinical, it is recognized that the foundation of all clinical strategies in preventive cardiology is the population approach to CVD prevention. The WHSF strongly endorses the World Health Report 2002 recommendations urging countries to adopt policies and programs to promote population-wide interventions such as reducing use of tobacco, reducing saturated fat in the national diet and salt in processed foods, encouraging higher consumption of fruits and vegetables, and encouraging weight reduction, and increase of exercise.
The ESC endorsed and collaborated with the initiatives and programs of different major international organizations (ie, WHO, European Union, international societies) in taking steps to implement measures at the population level, such as those for tobacco control established by the WHO Framework Convention for Tobacco,17 EU initiative on obesity,27 and the WHO Global Strategy on diet, physical activity, and health.18 The ESC Fourth Task Force fully endorses these initiatives and encourages health professionals of all countries to participate actively in the development and implementation of such national and international policies and community interventions.2
In the spirit of the Osaka declaration, the ESC has joined with the European Heart Network to engage with the European Union to promote a co-ordinated European approach to the prevention of cardiovascular diseases. The conclusions of the EU Council on Employment, Social Policy, Health and Consumer Affairs in June 2004 and the EU Heart Health Conference resulted in the Luxembourg Declaration in June 2005.28 The participants of the Heart Health conference agreed that necessary measures, giving priority to lifestyle interventions, should be considered by each Member State to reduce the burden of CVD. They agreed to raise awareness among European population of those characteristics associated with cardiovascular health:
- Avoidance of tobacco
- Adequate physical activity (at least 30 min/day)
- Healthy food choices
- Avoiding overweight
- Blood pressure below 140/90 mm Hg
- Blood cholesterol below 5 mmol/L (~190 mg/dL)
The Luxemburg Declaration defined the factors that are essential for implementation, and stressed the need for continued European Commission, Parliament and Council activity to promote a heart healthy Europe. A European Charter on Heart Health represents the combined efforts of the European Society of Cardiology, European Union and European Heart Network in close collaboration with the World Health Organisation Regional Office for Europe.29 The charter acknowledges that cardiovascular disease is the number one cause of death among men and women in Europe. The European Heart Charter affirms the characteristics associated with cardiovascular health defined in the Luxemburg declaration. It also categorises the major risk factors. The fourteen major European bodies associated with cardiovascular health signed the charter and agreed to:
- Implement the policies and measures agreed upon in high level European Political documents
- Advocate for and support the development and implementation of comprehensive health strategies as well as measures and policies on European, National, Regional and local level that promote cardiovascular health and prevent cardiovascular disease
- Build and strengthen dedicated heart health alliances in order to achieve the strongest possible political support for policy developments and co-ordination of actions to reduce the burden from cardiovascular disease
- Engage in education and empowerment of the public and patients by involving mass media and developing social marketing for raising awareness of CVD
The European Heart Charter also deals with the health promotion, the establishment of national strategies for detection and management of people at high CVD risk, and the endorsement of the European Guidelines on Cardiovascular Disease Prevention at country level. It is agreed to prioritize research on the effectiveness of policy and prevention interventions, to assess the current status of cardiovascular health including risk factor prevalences and to measure the progress at population and individual level.
GUIDELINES ON CVD PREVENTION
There is an international consensus among guidelines regarding the priorities and goals for CVD prevention, risk factor assessment and management, and use of drug therapies. However, this consensus mainly comes from guidelines developed in the United States, Europe, Australia, and New Zealand. For most of the developing countries in the Asia-Pacific region, Africa, and South America, there are few data on the prevalence and management of CVD and few published guidelines.1,2,30-37
In defining objectives for CVD prevention in clinical practice the priority is given to those patients who are at highest risk of developing CVD, rather than attempting to reach every adult in the population. Therefore, risk stratification is required. In the context of a comprehensive population strategy—to reduce tobacco smoking, encourage healthy food choices, and increase physical activity for the whole population—the medical priority is to focus on those with established atherosclerotic disease, and those apparently healthy individuals who are at high risk of developing atherosclerotic disease because of a combination of cardiovascular risk factors. The third priority is the close relatives of patients with early onset CVD and of healthy individuals at particularly high risk.
There is a strong agreement across international, continental, and national guidelines that patients with clinically established CVD have, at any level of a single risk factor or at any combination of risk factors, a much higher level of risk of recurrent disease than asymptomatic persons. As the modifiable risk factors continue to be important to the subsequent risk of atherosclerotic events in patients with clinically established CVD, management of lifestyle and other risk factors is of great importance in the proper care of such patients. These patients are recognized by cardiologists and other physicians as the top priority for prevention, and there is general agreement on the need for lifestyle intervention, blood pressure, cholesterol, and glucose management, and the use of prophylactic drug therapies: aspirin, beta-blockers, angiotesin converting enzyme (ACE) inhibitors/ angiotensin II receptor blockers (ARB), and lipid lowering drugs. There are some differences between guidelines on blood pressure and cholesterol goals for patients with CVD, but this is of practical importance only to a small minority of patients.
For healthy individuals, there is also agreement across international and national guidelines on the principle of taking the decision to treat blood pressure or lipids on absolute multifactorial risk of CVD. As CVD is multifactorial in its origins, it is important, in estimating the risk of apparently healthy individuals developing CVD, to consider all risk factors simultaneously. Traditionally, risk factor guidelines have been concerned with unifactorial assessment—in the management of hypertension or hyperlipidaemia—and this has resulted in undue emphasis being placed on individually high risk factors rather than the overall level of risk based on all factors taken together. In practice, clustering of risk factors will have a multiplicative effect and an individual with a number of modest risk factors may be at greater risk than someone with one very high risk factor. Absolute risk of CVD helps the physician to target preventive measures to those at highest risk and who are most likely to benefit. However, the practical application of this principle differs between guidelines in terms of the method of risk calculation, the absolute level of risk at which to intervene, and the risk factor thresholds themselves. All of these differences should be resolved at a national level by taking account of the scientific evidence and the resources available to deliver effective multifactorial intervention.
The advantages of a multifactorial approach to treatment in primary prevention of CVD are:
- Concept of continuous risk replaces the dichotomous classification of risk factors
- Level of absolute (multifactorial) risk for which treatment is given is not fixed
- Treatment is targeted at those with the highest absolute CVD risk
- Benefit is potentially greatest in those at high multifactorial risk
- Avoids treatment of single risk factors in those at low multifactorial risk
The disadvantage of a multifactorial approach to treatment in primary prevention of CVD is that treatment is concentrated in the older population unless the effect of lifetime exposure is taken into account.
The calculation of risk needs to be adjusted by the physician who takes account of other clinical factors. For example, clinical evidence of other cardiovascular risk factors, end organ damage, such as hypertensive retinopathy, or a family history of premature coronary heart disease (CHD) both increase cardiovascular risk, but may not be part of formal risk calculation. So the physician has to look at the complete clinical picture when judging an individual's absolute risk of developing cardiovascular disease (CVD) over time.
Calculation of Cardiovascular Disease Risk
Cardiovascular risk calculation is now incorporated into international and national guidelines for the prevention of CVD. Practical methods—tables, charts, and computer programs—have been developed for the assessment of an individual's absolute risk of developing CVD on the basis of risk functions derived from prospective epidemiological studies. The majority of these methods are based on the risk function derived from the Framingham Study.38,39 This function has been widely used to predict CHD and CVD risk because it is the classical epidemiological study of risk and CVD and the data are in the public domain. Simplified forms of the Framingham risk function have been used in the New Zealand,30,31 European,32-34 UK,35 and WHO guidelines1 for prevention of CHD, to target treatment at those at highest absolute risk. Framingham risk scoring has also been used in the National Cholesterol Education Program Adult Treatment Panel III (NCEP- ATP III) risk assessment for developing CHD.36 However, there were several concerns about using the risk function from Framingham study for estimating of the total CVD risk in Europe. Firstly, the charts were derived from American data and the application to the European populations was uncertain. Secondly the dataset was fairly small. The European Joint Task Forces were aware of the limitations of the Framingham based coronary risk chart, so a special project called SCORE (Systematic COronary Risk Estimation), funded by European Union, was set up to address these concerns and were recommended in the Joint European Societies Guidelines in 2003 and 2007.2,37,40
Threshold for Interventions
The appropriate threshold of an individual's total risk at which intensive lifestyle interventions and drug treatment are initiated depends on the availability of resources and the impact of specific interventions. The cost-effectiveness of pharmacological treatment for high blood pressure and blood cholesterol depends on the total cardiovascular risk of the individual before treatment; long-term drug treatment is justified only in high-risk individuals. If resources allow, the target population can be expanded to include those with moderate levels of risk. People with low levels of risk will benefit from population-based public health strategies and, if resources allow, professional assistance to make behavioural changes.
The 2007 WHO guidelines on prevention of cardiovascular disease provide guidance to policy-makers and health care workers on how to target individuals at high risk of developing CVD, at all levels of the health system and in different resource settings, using evidence-based and cost-effective preventive approaches.1
In all populations it is essential that the high-risk approach elaborated in this document is complemented by population-wide public health strategies. Although cardiovascular events are less likely to occur in people with low levels of risk, no level of risk can be considered "safe." Without population-wide public health prevention efforts, CVD events will continue to occur in people with low and moderate levels of risk, who are the majority in any population.
Furthermore, public health approaches can effectively slow down the development of atherosclerosis (and also reduce the incidence of some cancers and chronic respiratory diseases) in young people, thereby reducing the likelihood of future epidemics of CVD, such as were seen in 1960-1990 in most high-income countries. Population-wide strategies will also support lifestyle modification in those at high risk. The extent to which one strategy is emphasized over the other depends on achievable effectiveness, cost-effectiveness and resource considerations.
Ministries of health have the difficult task of setting a risk threshold for treatment to match resources according to the 10-year total CVD risk: a) high-resource setting: 20%; b) medium-resource setting: 30%; and c) low-resource setting: 40%.1
Adoption of a high (40%) threshold for 10-year CVD risk in a population might seem economical; however, this would deny most of the population the opportunity to prevent or delay development of CVD. Nevertheless, in low-income countries, lowering the threshold below 40% may not be feasible because of resource limitations.
Risk Prediction Charts
The risk charts and tables produced use different age categories, duration of risk assessment and risk factor profiles. The risk prediction charts and the accompanying recommendations can be used by health care professionals to match the intensity of risk factor management with the likelihood of cardiovascular disease events. The charts can also be used to explain to patients the likely impact of interventions on their individual risk of developing cardiovascular disease. This approach may motivate patients to change their behaviour. The use of charts will help health care professionals to focus their limited time on those who stand to benefit the most.
The WHO/ISH (International Society of Hypertension) cardiovascular risk prediction charts are available for each WHO subregion (and country) (http://www.who. int/bookorders).
The charts have been generated from the best available data, using a modelling approach, with age, sex, smoking, blood pressure, blood cholesterol, and presence of diabetes as clinical entry points for overall management of cardiovascular risk.
Separate charts have been developed for assessment of cardiovascular risk in patients with type 2 diabetes. In many low-resource settings, there are no facilities for cholesterol assay, although it is often feasible to check urine sugar as a surrogate measure for diabetes. Therefore, there are risk prediction charts that do not use cholesterol, but only age, sex, smoking, systolic blood pressure, and presence or absence of diabetes to predict cardiovascular risk.
THE SCORE EUROPEAN PROJECT
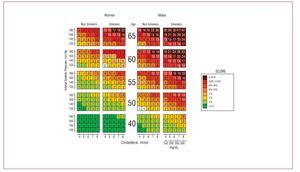
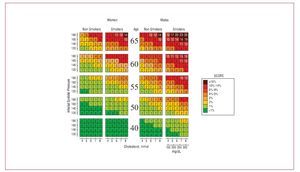
SCORE is a risk estimation system, based on data from 12 European cohort studies and includes 205178 subjects examined at baseline between 1970 and 1988 with 2.7 million years of follow-up and 7934 cardiovascular deaths.2,37,40 The SCORE system estimates the 10 year risk of a first fatal atherosclerotic event, whether heart attack, stroke, aneurysm of the aorta or other (Figures 1 and 2).
Figure 1. SCORE charts for risk of fatal cardiovascular disease in 10 years for populations with high risk of cardiovascular disease. (Reproduced with permission of de Backer G et al37.)
Figure 2. SCORE charts. Risk of fatal cardiovascular disease in 10 years for populations with low risk of cardiovascular disease. (Reproduced with permission of de Backer G et al37.)
The main features of the SCORE risk prediction system are:
- The prediction is based on total cardiovascular deaths rather than the combination of non-fatal and fatal coronary events. Non-CHD cardiovascular mortality is especially important because it represents a greater proportion of all cardiovascular risk in European regions with low rates of CHD. An absolute fatal CVD risk ≥5% from SCORE is equivalent to a CHD event risk ≥20% based on the Framingham function
- A SCORE risk function has been calculated for high-and low-risk European regions. The low risk charts should be recommended for use in Belgium, France, Greece, Italy, Luxembourg, Spain, Switzerland, and Portugal and also in countries which have recently experienced a substantial lowering of the CV mortality rates. The high risk charts should be recommended in all other countries of Europe. (Updated, recalibrated charts are now available for Belgium, Germany, Greece, The Netherlands, Poland, Spain, and Sweden)
- The risk is displayed as a percentage (probability of fatal CVD over a 10 year period) rather than a broad risk category
- The cardiovascular risk is calculated in 2 ways: one based on total cholesterol and the other on the total cholesterol/HDL-cholesterol ratio
A fatal CVD risk ≥5% based on SCORE is considered to be sufficiently high to justify intensive lifestyle intervention and, where appropriate, the use of drug therapies.
Risk will be higher than indicated in the charts in:
- Sedentary subjects and those with central obesity
- Socially deprived individuals
- Individuals with diabetes: re-analysis of the SCORE data base indicates that those with known diabetes are at greatly increased risk; 5 times higher in women and 3 times higher in men
- Individuals with low HDL cholesterol, increased triglycerides, fibrinogen, apolipoprotein B and lipoprotein (a) levels and perhaps increased high-sensitivity CRP and homocysteine levels
- Asymptomatic individuals with pre-clinical evidence of atherosclerosis, for example on ultrasonography
HeartScore® (available from: http://www.escardio.org) is a comprehensive computer-based CVD risk estimation and management program for prevention of CVD. It is an electronic, interactive version of SCORE. HeartScore® is a risk prediction and management web-based program aimed at supporting clinicians in optimising individual cardiovascular risk reduction. The HeartScore® web-based program is based on the internet technology and uses the risk function and data from the SCORE project.
In summary, the causes of CVD are the same across the world, but the approaches to its prevention at a societal or individual level differ between countries for cultural, social, economical, and medical reasons. Every country should implement national clinical guidelines for CVD prevention. Developing countries need to re-prioritise their health systems and use the international principles to develop effective strategy to control the burden of CVD. Since cardiovascular diseases are a global problem, the national and international societies of cardiology need to collaborate in defining the strategies for cardiovascular prevention. Population and high-risk strategies are both necessary and complement each other and the balance between them will depend on the absolute level of risk and its distribution in each specific population.
Seccion Sponsored by Laboratorio Dr Esteve
Correspondence: Kornelia Kotseva, MD, PhD, FESC.
National Heart and Lung Institute, Imperial College London, Charing Cross Hospital.
Fulham Palace Road, London W6 8RF, UK.
E-mail: k.kotseva@imperial.ac.uk