Visual angiographic assessment continues to be used when decisions are made on whether to revascularize ambiguous coronary lesions. Multiple factors, other than the degree of stenosis, have been associated with the functional significance of a coronary lesion. The aim of this study was to investigate the ability of interventionists to visually predict the functional significance of a coronary lesion and the clinical and angiographic characteristics associated with errors in prediction.
MethodsWe conducted a concordance study of the functional significance of coronary lesions predicted by experienced interventionists and fractional flow reserve values measured by intracoronary pressure wire in 665 intermediate lesions (40%-70% diameter stenosis) in 587 patients. We determined which factors were independently associated with errors in prediction.
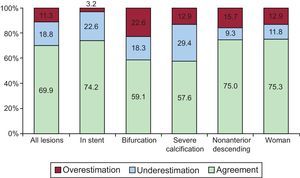
ResultsThere was disagreement between the predicted fractional flow reserve value of ≤ 0.80 and the observed value in 30.1% of the lesions (overestimation: 11.3%; underestimation, 18.8%). Stent location in an artery other than the anterior descending artery or in a bifurcation was associated with overestimation. Male sex, severe calcification, and a greater myocardial territory distal to the lesion were significantly associated with the functional significance of the underestimated lesion.
ConclusionsEven when taking into account angiographic and clinical characteristics, there is a high rate of disagreement between visual estimation and direct measurement of intermediate coronary stenosis in relation to its functional significance. Specific angiographic and clinical characteristics are associated with an increased tendency to overestimate or underestimate the significance of lesions.
Keywords
Although the main purpose of coronary revascularization is to treat myocardial ischemia, the degree of angiographic stenosis is used as the main parameter to guide decisions on whether to revascularize a lesion1–3 or to determine the presence of restenosis after treatment. The significance of a coronary lesion is classically defined by the degree of angiographic stenosis, which is obtained by dividing the minimal lumen diameter by the reference diameter in the projection showing the greatest stenosis.4,5 Invasive measurement of fractional flow reserve (FFR) has recently become established as the method of choice to determine the functional significance of coronary lesions, especially when their potential to produce ischemia is ambiguous.4,5 Several studies have shown the limitations of angiography to define the functional significance of a lesion.6–9 These limitations may be due to the difficulty of determining the true degree of stenosis in the presence of certain angiographic characteristics (curvature, calcification, bifurcations, ostial location, etc); another factor is that the functional significance of a lesion is determined by other factors that add to the degree of stenosis. The FFR across a specific lesion is affected, among others factors, by the size of the myocardial territory perfused by the vessel with the lesion,10 lesion length,11,12 the presence of collateral vessels,13,14 diffuse disease of the distal bed, or the state of the microcirculation.15,16
Although several studies have found poor correlations between the functional significance of a lesion obtained by visual assessment and by FFR,6–9,17 few studies have analyzed the factors associated with this discrepancy. The aim of the present study was to investigate the clinical and angiographic variables that could be associated with a greater degree of error when the functional significance of a coronary lesion is assessed by angiography.
METHODSDesign and Study PatientsWe conducted a retrospective observational study of a historic cohort of patients referred to a cardiac catheterization laboratory for coronary angiography for suspected coronary disease between January 1, 2008 and May 31, 2012. The patients were evaluated for revascularization by measuring the FFR across an intermediate coronary lesion (40%-70% diameter stenosis by visual estimation) using a pressure wire. We excluded patients with lesions > 20% in a segment distal or proximal to the target lesion. The FFR was not measured in vessels that perfused akinetic or previously infarcted territory. In patients with acute coronary syndrome, the FFR was only measured in nonculprit vessels.
ProcedureAll procedures were performed according to the usual protocol of the center conducting the study. After the decision was made to measure the FFR, the diagnostic catheter used for angiography was replaced by a 6-Fr guide catheter. This catheter was used to repeat the projections providing the best visualization of the lesions, with greater visual stenosis and without overlapping branches or loss of length because of curvature. All patients received 100 IU/kg intravenous sodium heparin before the procedure if not previously administered. Functional evaluation was performed with a 0.014-inch intracoronary pressure wire (Pressure Wire, Certus or Airis, Radi Medical Systems; Uppsala, Sweden, or PrimeWire Prestige Pressure Guide Wire, Volcano Corp.; San Diego, California, United States). The pressure wire was calibrated externally and then advanced to the distal end of the guide catheter while equalizing the pressures according to the system used to measure the FFR. After administration of 200 μg to 300 μg intracoronary nitroglycerin, the guide was advanced until the sensor was at least 20 mm distal to the lesion. We followed the standard procedure used in our hospital to obtain the FFR by administering 300 μg to 1200 μg intracoronary adenosine, while taking particular care to avoid wedging the catheter in the coronary ostium after bolus injection of the drug. The beat-to-beat ratio of the mean aortic pressure at the end of the guide catheter and the pressure distal to the lesion, obtained via the pressure wire under maximum hyperemia, were used to measure the FFR. We measured the FFR at least 3 times and used the lowest measurement. We successively administered 300 μg, 600 μg and 1200 μg intracoronary adenosine whenever the previous dose failed to produce a period of asystole ≥ 6 s.
The decision to revascularize was left to the operator's discretion based on the data obtained in the angiographic and functional study.
Angiographic VariablesIn our hospital, the routine method to obtain the FFR includes obtaining at least 1 projection that provides the best visualization of the lesion using the guide catheter, after the administration of intracoronary nitroglycerin. The diagnostic angiographic sequences of each procedure were separated from those obtained during the intervention (when applicable). The observers were only provided with diagnostic images and were blinded to the result of the FFR study when performing the digital quantification of lesion stenosis. Data were collected on the following variables: severe calcification (multiple opacification visible in more than 1 projection covering the entire vessel lumen at the site of the lesion); bifurcation (presence of a > 15-mm side branch originating at the site of the lesion); angulation > 45° (target lesion in a segment with angulation > 45°); ostial location (lesion at the origin of the vessel in the aorta); perfused myocardial territory (Duke jeopardy score18,19); and location of the lesion in the stent.
Digital quantification was performed using the QAngio XA version 7.1.43.0 postprocessing software package (Medis Medical Imaging Systems; Leiden, The Netherlands).
The lesions were analyzed by 2 experienced interventional cardiologists (more than 1000 coronary interventions using a pressure wire/measuring the FRR). One of them analyzed the lesions twice (OBS1A and OBS1B, with a 4-month interval between assessments), and the other analyzed them once (OBS2). They predicted whether the result of the pressure wire study was positive (FFR ≤ 0.80). The 2 observers were blinded to the previous predictions, the assessments made by the other, and the FFR results.
Based on their previous experience and published scientific evidence, the 2 observers took into account not only the degree of stenosis when making their predictions but also other parameters that have been associated with the FFR.16 In cases of disagreement, the mode of the 3 predictions was used. Overestimation was defined by a predicted FFR ≤ 0.80 vs a measured FFR > 0.80. Underestimation was defined by a predicted FFR > 0.80 vs a measured FFR ≤ 0.8. Disagreement was defined by the underestimation or overestimation of the FFR. We analyzed the factors associated with disagreement, overestimation, or underestimation.
Statistical AnalysisAll quantitative variables are expressed as mean±standard deviation and were compared using the Student t test. Qualitative variables are expressed as absolute values (percentages) and were compared using the chi-squared test. Logistic regression models were used to analyze the angiographic and clinical variables associated with an observed FFR ≤ 0.80, an estimated FFR ≤ 0.80, and disagreement (overestimation and underestimation) between the predicted and observed functional significance of the lesions. A P-value of <.5 was used as a cutoff for statistical significance. The Hosmer-Lemeshow test and the area under the ROC (receiver operating characteristic) curve were used to assess the model's goodness-of-fit and predictive power, respectively. All analyses were conducted using the SPSS 20.0 statistical package for Windows (SPSS Inc.; Chicago, Illinois, United States). Although this study compared 2 diagnostic tests, rather than assessing the reliability of 1 diagnostic test, the recommendations of the STARD initiative in data presentation were followed as closely as possible.20
RESULTSWe studied 665 lesions in 587 patients. Table 1 shows the clinical and angiographic characteristics of the patients. Coronary angiography was performed in 56% of the patients in the setting of acute coronary syndrome. In total, 58% of the lesions were located in the anterior descending coronary artery, 26% had severe calcification, and 9% were in-stent restenosis. An FFR of ≤ 0.80 was obtained in 29.9% of the lesions (199).
Baseline Characteristics of the Patients
| Clinical characteristics of the patients (n=587) | |
| Age, y | 67.9±10.6 |
| Women | 162 (27.6) |
| Hypertension | 438 (74.6) |
| Diabetes mellitus | 245 (41.7) |
| Smoking | 279 (47.5) |
| Hyperlipidemia | 316 (53.8) |
| Previous infarction | 132 (22.5) |
| Previous coronary revascularization | 158 (26.9) |
| Percutaneous | 138 (23.5) |
| Surgical | 6 (1.1) |
| Prior stroke | 46 (7.8) |
| Indication for coronary angiography | |
| STEACS | 46 (7.8) |
| NSTEACS | 287 (48.9) |
| Stable angina/silent ischemia | 254 (43.3) |
| Angiographic characteristics of the lesions (n=665) | |
| Target lesion | |
| Anterior descending | 386 (58.0) |
| Circumflex | 135 (20.3) |
| Right coronary | 136 (20.5) |
| Left main coronary | 7 (1.1) |
| Angulation > 45° | 37 (5.6) |
| Calcification | 170 (25.6) |
| Ostium | 58 (8.7) |
| Bifurcation | 35 (17.6) |
| Duke jeopardy score | 3.54±1.50 |
| Location in the stent | 62 (9.3) |
| Stenosis, % | 50.3±9.7 |
| Length, mm | 14.0±7.2 |
| Reference diameter, mm | 2.7±0.6 |
| FFR value | 0.83±0.09 |
| FFR ≤ 0.80 | 199 (29.9) |
FFR, fractional flow reserve; NSTEACS, non—ST-segment elevation acute coronary syndrome; STEACS, ST-segment elevation acute coronary syndrome.
Values are expressed as No. (%) or mean±standard deviation.
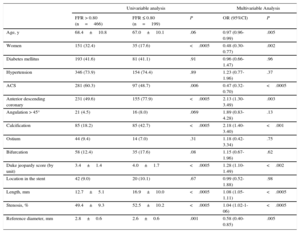
Table 2 shows the distribution of the clinical and angiographic variables according to the FFR value. After adjustment for other variables, age, male sex, absence of acute coronary syndrome, the presence of calcification, target segment with an angulation > 45°, anterior descending coronary artery location, a greater degree of stenosis, greater length, smaller reference diameter, and greater territory distal to the target lesion were associated with FFR ≤ 0.80 (Table 2, right).
Univariable Analysis of the Observed Fractional Flow Reserve ≤ 0.80 or > 0.80 and Logistic Regression Analysis
| Univariable analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|
| FFR > 0.80 (n=466) | FFR ≤ 0.80 (n=199) | P | OR (95%CI) | P | |
| Age, y | 68.4±10.8 | 67.0±10.1 | .06 | 0.97 (0.96-0.99) | .005 |
| Women | 151 (32.4) | 35 (17.6) | <.0005 | 0.48 (0.30-0.77) | .002 |
| Diabetes mellitus | 193 (41.6) | 81 (41.1) | .91 | 0.96 (0.66-1.47) | .96 |
| Hypertension | 346 (73.9) | 154 (74.4) | .89 | 1.23 (0.77-1.96) | .37 |
| ACS | 281 (60.3) | 97 (48.7) | .006 | 0.47 (0.32-0.70) | <.0005 |
| Anterior descending coronary | 231 (49.6) | 155 (77.9) | <.0005 | 2.13 (1.30-3.49) | .003 |
| Angulation > 45° | 21 (4.5) | 16 (8.0) | .069 | 1.89 (0.83-4.28) | .13 |
| Calcification | 85 (18.2) | 85 (42.7) | <.0005 | 2.18 (1.40-3.40) | <.001 |
| Ostium | 44 (9.4) | 14 (7.0) | .31 | 1.18 (0.42-3.34) | .75 |
| Bifurcation | 58 (12.4) | 35 (17.6) | .08 | 1.15 (0.67-1.96) | .62 |
| Duke jeopardy score (by unit) | 3.4±1.4 | 4.0±1.7 | <.0005 | 1.28 (1.10-1.49) | <.002 |
| Location in the stent | 42 (9.0) | 20 (10.1) | .67 | 0.99 (0.52-1.88) | .98 |
| Length, mm | 12.7±5.1 | 16.9±10.0 | <.0005 | 1.08 (1.05-1.11) | <.0005 |
| Stenosis, % | 49.4±9.3 | 52.5±10.2 | <.0005 | 1.04 (1.02-1-06) | <.0005 |
| Reference diameter, mm | 2.8±0.6 | 2.6±0.6 | .001 | 0.58 (0.40-0.85) | .005 |
95%CI, 95% confidence interval; ACS, acute coronary syndrome; FFR, fractional flow reserve; OR, odds ratio.
Values are expressed as No. (%) or mean±standard deviation. Hosmer-Lemeshow test: chi-squared=7.03; degrees of freedom, 8; significance, 0.53. Area under the receiver operating characteristic curve, 0.81 (range, 0.77-0.84; P<.0005)
In relation to the predicted FFR value ≤ 0.80, intraobserver agreement was 83% (κ=0.54±0.039; P<.0005) and interobserver agreement was 79.4% (κ=0.43±0.041; P<.0005).
Agreement between the FFR value estimated by the observers (the statistical mode of the estimates made by OBS1A, OBS1B, and OBS2) and the measured FFR value was 69.9% (overestimation, 11.3%; underestimation, 18.8%). Visual estimation of FFR ≤ 0.80 had a sensitivity of 37.2% (95% confidence interval [95%CI], 0.30-0.44), specificity of 83.9% (95%CI, 0.81-0.87), positive predictive value of 49.7% (95%CI, 0.42-0.58), and negative predictive value of 75.8% (95%CI, 0.72-0.79). Observer agreement (OBS1A, OBS1B, and OBS2) on FFR ≤ 0.80 was 67.1%, 67.0%, and 70.1%, respectively.
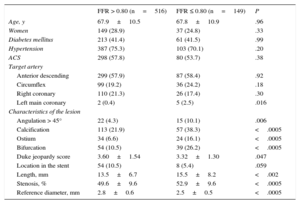
Table 3 shows the distribution of the clinical and angiographic variables according to the functional significance estimated by the observers.
Clinical and Angiographic Characteristics of the Lesions According to the Estimated Fractional Flow Reserve
| FFR > 0.80 (n=516) | FFR ≤ 0.80 (n=149) | P | |
|---|---|---|---|
| Age, y | 67.9±10.5 | 67.8±10.9 | .96 |
| Women | 149 (28.9) | 37 (24.8) | .33 |
| Diabetes mellitus | 213 (41.4) | 61 (41.5) | .99 |
| Hypertension | 387 (75.3) | 103 (70.1) | .20 |
| ACS | 298 (57.8) | 80 (53.7) | .38 |
| Target artery | |||
| Anterior descending | 299 (57.9) | 87 (58.4) | .92 |
| Circumflex | 99 (19.2) | 36 (24.2) | .18 |
| Right coronary | 110 (21.3) | 26 (17.4) | .30 |
| Left main coronary | 2 (0.4) | 5 (2.5) | .016 |
| Characteristics of the lesion | |||
| Angulation > 45° | 22 (4.3) | 15 (10.1) | .006 |
| Calcification | 113 (21.9) | 57 (38.3) | <.0005 |
| Ostium | 34 (6.6) | 24 (16.1) | <.0005 |
| Bifurcation | 54 (10.5) | 39 (26.2) | <.0005 |
| Duke jeopardy score | 3.60±1.54 | 3.32±1.30 | .047 |
| Location in the stent | 54 (10.5) | 8 (5.4) | .059 |
| Length, mm | 13.5±6.7 | 15.5±8.2 | <.002 |
| Stenosis, % | 49.6±9.6 | 52.9±9.6 | <.0005 |
| Reference diameter, mm | 2.8±0.6 | 2.5±0.5 | <.0005 |
ACS, acute coronary syndrome; FFR, fractional flow reserve.
Values are expressed as No. (%) or mean±standard deviation.
Univariable analysis showed that the degree of angiographic stenosis, a smaller reference diameter, calcification, angle of the bifurcation, and an ostial location were associated with an estimated FFR ≤ 0.80. In the unadjusted analysis, the Duke jeopardy score, paradoxically, showed an inverse association with a higher estimated FFR ≤ 0.80 (Duke jeopardy score, 3.60 in lesions with an expected FFR > 0.80 vs 3.32 with and estimated FFR ≤ 0.80; P=0.047).
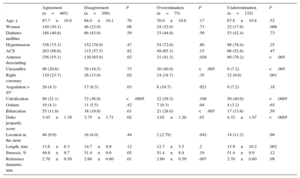
Functional significance was overestimated in 75 lesions (16% of which had an FFR > 0.80) and underestimated in 125 lesions (62.8% of which had an FFR ≤ 0.80). Table 4 shows the distribution of the variables according to agreement, underestimation, or overestimation. Severe calcification, lesion length, and lesion location in the right coronary artery were associated with underestimating the significance of the lesion. Location of the lesion in the stent, ostium, or bifurcation, and angulation were associated with overestimation.
Clinical and Angiographic Characteristics of the Lesions According to Agreement on the Functional Significance of the Lesion Estimated by Visual Assessment and Observed Fractional Flow Reserve
| Agreement (n=465) | Disagreement (n=200) | P | Overestimation (n=75) | P | Underestimation (n=125) | P | |
|---|---|---|---|---|---|---|---|
| Age, y | 67.7±10.8 | 68.0±10.1 | .76 | 70.0±10.8 | .17 | 67.8±10.8 | .52 |
| Women | 140 (30.1) | 46 (23.0) | .06 | 24 (32.0) | .73 | 22 (17.6) | .006 |
| Diabetes mellitus | 188 (40.8) | 86 (43.0) | .59 | 33 (44.0) | .59 | 53 (42.4) | .73 |
| Hypertension | 338 (73.3) | 152 (76.0) | .47 | 54 (72.0) | .80 | 98 (78.4) | .25 |
| ACS | 263 (56.6) | 115 (57.5) | .82 | 49 (65.3) | .15 | 66 (52.8) | .47 |
| Anterior descending | 256 (55.1) | 130 (65.0) | .02 | 31 (41.3) | .028 | 99 (79.2) | <.005 |
| Circumflex | 96 (20.6) | 39 (19.5) | .73 | 30 (40.0) | <.005 | 9 (7.2) | <.005 |
| Right coronary | 110 (23.7) | 26 (13.0) | .02 | 14 (18.7) | .35 | 12 (9.6) | .001 |
| Angulation > 45° | 20 (4.3) | 17 (8.5) | .03 | 8 (10.7) | .021 | 9 (7.2) | .18 |
| Calcification | 98 (21.1) | 72 (36.0) | <.0005 | 22 (29.3) | .108 | 50 (40.0) | <.0005 |
| Ostium | 19 (4.1) | 11 (5.5) | .42 | 7 (9.3) | .04 | 4 (3.2) | .65 |
| Bifurcation | 55 (11.8) | 38 (19.0) | .01 | 21 (28.0) | <.005 | 17 (13.6) | .59 |
| Duke jeopardy score | 3.45±1.38 | 3.75±1.71 | .02 | 3.01±1.20 | .01 | 4.32±1.97 | <.0005 |
| Location in the stent | 46 (9.9) | 16 (8.0) | .44 | 2 (2.79) | .042 | 14 (11.2) | .66 |
| Length, mm | 13.6±6.3 | 14.7±8.9 | .12 | 12.7±5.5 | .2 | 15.9±10.2 | .002 |
| Stenosis, % | 49.8±9.7 | 51.4±9.6 | .05 | 51.4±8.9 | .19 | 51.4±9.9 | .12 |
| Reference diameter, mm | 2.70±0.59 | 2.60±0.60 | .01 | 2.60±0.59 | .007 | 2.70±0.60 | .09 |
ACS, acute coronary syndrome; FFR, fractional flow reserve.
Values are expressed as No. (%) or mean±standard deviation.
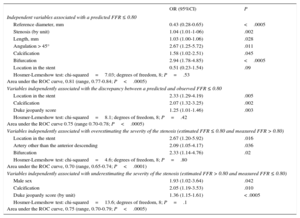
Multivariable analysis showed that severe angiographic calcification, angulation > 45° in the target segment, bifurcation location, greater length, greater diameter stenosis, and a smaller reference diameter were associated with estimation of the functional significance of the lesion (Table 5).
Logistic Regression Analysis of the Variables Associated with a Predicted Fractional Flow Reserve ≤ 0.80 and Disagreement (Underestimation or Overestimation) on the Observed Fractional Flow Reserve
| OR (95%CI) | P | |
|---|---|---|
| Independent variables associated with a predicted FFR ≤ 0.80 | ||
| Reference diameter, mm | 0.43 (0.28-0.65) | <.0005 |
| Stenosis (by unit) | 1.04 (1.01-1-06) | .002 |
| Length, mm | 1.03 (1.00-1.06) | .028 |
| Angulation > 45° | 2.67 (1.25-5.72) | .011 |
| Calcification | 1.58 (1.02-2.51) | .045 |
| Bifurcation | 2.94 (1.78-4.85) | <.0005 |
| Location in the stent | 0.51 (0.23-1.54) | .09 |
| Hosmer-Lemeshow test: chi-squared=7.03; degrees of freedom, 8; P=.53 Area under the ROC curve, 0.81 (range, 0.77-0.84; P<.0005) | ||
| Variables independently associated with the discrepancy between a predicted and observed FFR ≤ 0.80 | ||
| Location in the stent | 2.33 (1.29-4.19) | .005 |
| Calcification | 2.07 (1.32-3.25) | .002 |
| Duke jeopardy score | 1.25 (1.01-1.46) | .003 |
| Hosmer-Lemeshow test: chi-squared=8.1; degrees of freedom, 8; P=.42 Area under the ROC curve 0.75 (range 0.70-0.78; P<.0005) | ||
| Variables independently associated with overestimating the severity of the stenosis (estimated FFR ≤ 0.80 and measured FFR > 0.80) | ||
| Location in the stent | 2.67 (1.20-5.92) | .016 |
| Artery other than the anterior descending | 2.09 (1.05-4.17) | .036 |
| Bifurcation | 2.33 (1.14-4.76) | .02 |
| Hosmer-Lemeshow test: chi-squared=4.6; degrees of freedom, 8; P=.80 Area under the ROC curve, 0.70 (range, 0.65-0.74; P<.0001) | ||
| Variables independently associated with underestimating the severity of the stenosis (estimated FFR > 0.80 and measured FFR ≤ 0.80) | ||
| Male sex | 1.93 (1.02-3.64) | .042 |
| Calcification | 2.05 (1.19-3.53) | .010 |
| Duke jeopardy score (by unit) | 1.36 (1.15-1.61) | < .0005 |
| Hosmer-Lemeshow test: chi-squared=13.6; degrees of freedom, 8; P=.1 Area under the ROC curve, 0.75 (range, 0.70-0.79; P<.0005) | ||
95%CI, 95% confidence interval; FFR, fractional flow reserve; OR, odds ratio; ROC: receiver operating characteristic.
In all cases, adjustments were made by age, sex, hypertension, diabetes mellitus, acute coronary syndrome, anterior descending artery location, reference diameter, lesion length, degree of stenosis, stent location, bifurcation location, ostial location, angulation > 45°, calcification, and Duke jeopardy score.
After adjustment for other variables, the variables independently associated with incorrectly classifying the functional significance of the lesion by visual estimation were stent location, calcification, and the size of the coronary territory distal to target lesion (Table 5).
The variables associated with overestimating the functional significance of the lesions were location in the stent, in an artery other than the anterior descending artery, and in a bifurcation (Table 5).
Male sex, a larger myocardial territory perfused by the vessel with the lesion, and severe calcification were significantly and independently associated with underestimating the functional significance of the lesion by visual estimation (Table 5).
DISCUSSIONPrevious studies have shown a weak correlation between the angiographic quantification (visual or automated) of coronary lesions and their functional significance.6,9 This study is the first to analyze the variables associated with errors (both overestimation and underestimation) in the visual assessment of the functional significance of coronary lesions. The specialists conducting the visual estimation are not only experienced in interventional cardiology, but also have specific experience in the use of FFR for making decisions and in taking into account the degree of stenosis of the lesion and other factors that determine the functional significance of coronary lesions. This study shows that even interventionists who are experienced in the invasive functional assessment of lesions can fail to visually predict the functional significance of lesions.
Overestimation of the functional significance of lesions was associated with the location of the lesion in an artery other than the anterior descending artery, in the stent, and in a bifurcation. Underestimation was associated with male sex, severe calcification, and greater coronary area distal to the lesion (Figure).
The results of this study are consistent with those obtained in previous studies regarding low intraobserver and interobserver agreement in the visual assessment of the severity of intermediate coronary lesions. Matching values were higher than those of other studies based solely on the degree of stenosis.6,8 Despite being members of the same intervention team and using similar criteria for the estimations, κ<0.6 was obtained, which indicates the low reliability of the visual assessment of lesions.
Invasive measurement of FFR addresses characteristics of the coronary lesion apart from the degree of stenosis alone. Frequent use of the FFR in the cardiac catheterization laboratory may have an “instructive” effect that would lead the interventionist to modify the assessment of the significance of the lesion by taking into account aspects such as the lesion length, disease of the distal bed, or the size of the myocardium distal to the lesion, in addition to its degree of stenosis. In a recent study, Park et al.9 used the degree of angiographic stenosis (52% diameter stenosis) as the only classification parameter. They found an agreement of 66% with a sensitivity of 66%, a specificity of 67%, and positive and negative predictive values of 48% and 81%, respectively9. We used multiple clinical and angiographic parameters to visually estimate the functional significance of the lesion and observed a slightly higher agreement (70%), lower sensitivity, and greater specificity.
The percentage of lesions with an FFR > 0.80 considered significant by visual estimation was significantly lower than that observed by Park et al. (16% vs 57%). In contrast, a much higher percentage of lesions with an FFR ≤ 0.80 were visually classified as functionally nonsignificant (63% vs 16%). The frequent use of the FFR in intermediate lesions probably leads to the application of a “functional approach” to their assessment, without invasive measurement, which would lead to a more conservative assessment when considering a lesion functionally significant.
Angiographic Characteristics Associated With Visually Overestimating a LesionTogether with the inability of angiography to predict the functional significance of coronary lesions, our study shows that certain angiographic characteristics of the lesion may be associated with underestimating or overestimating the significance of the stenosis. If these angiographic characteristics are present in an angiographically intermediate stenosis, the probability of error when decisions are made on whether to revascularize without a functional study can be even greater than in the general population.
In our study, moderate in-stent restenosis (40%-70% stenosis) was the factor most strongly associated with overestimating the significance of the lesion. The presence of bare-metal stents makes it difficult to determine the edges of the vessel lumen, which can lead to underestimation of its diameter and overestimation of the degree of restenosis. Although previous studies have demonstrated the limitations of angiography in assessing in-stent restenosis,21,22 recent clinical trials have continued to use the degree of angiographic stenosis to determine restenosis or to decide whether to revascularize the treated lesion.23–25 The use of FFR for the functional assessment of the lesion during follow-up in these studies could have led to fewer restenosis events being assigned to patients undergoing percutaneous coronary intervention.
The location of the lesion in an artery other than the anterior descending artery was one of the variables associated with overestimating the functional significance of the lesion. In the multivariable analysis, an adjustment was made for the myocardial territory perfused by the artery with the lesion. This adjustment may have been insufficient, such that the observed overestimation could have been due to a smaller myocardial area in lesions in locations other than the anterior descending artery with a greater FFR value for the same diameter stenosis value. This possibility is consistent with the finding of an association between a larger myocardial territory distal to the lesion and underestimating the functional significance of the lesion. Although the researchers were aware of the effect of perfused myocardial territory on the FFR value for a given lesion, the angiographic characteristics of the lesion continued to take precedence over the other characteristics when estimates were made on its functional significance. The location of the lesion in a bifurcation was also associated with the functional overestimation of the stenosis. Several studies have demonstrated the difficulty of assessing these lesions angiographically and have shown that less functional significance is found when the FFR is used than might be expected by the degree of stenosis observed both before and after treatment of the lesion.26,27
Angiographic Characteristics Associated With Visually Underestimating a LesionMale sex and severe calcification were associated with underestimation of the functional significance of lesions. As the researchers were blinded to the sex of the patients when assessing the lesions, they could not have taken this variable into account in their estimates. Our findings are in line with those of several studies that have found an association between female sex and a greater FFR value for the same degree of stenosis in men and women.28–30
Calcification hampers the visual and automated angiographic assessment of stenosis. In this study, in contrast to in-stent restenosis, calcification was associated with underestimating the significance of the lesion. Increased radiodensity due to increased vessel thickness can contribute to overestimating lumen diameter, which would lead to systematic errors in visual assessment. Moreover, coronary calcification can be a marker of more extensive and diffuse disease and could lead to diseased coronary segments being used as a reference, and thus lead to underestimation of the degree of stenosis or lesion length.
LimitationsThis study was conducted at a single hospital. Although the researchers who visually assessed the lesions were blind to the results of the FFR study and to each other's estimates, local factors may have influenced estimation of the functional significance of the lesions. The generalizability of our findings is supported by the low interobserver agreement found in this study, which is similar to that found other published studies, and agreement with the literature regarding the variables associated with the predictions. The use of the mode in the 3 estimates gave more weight to the observations of OBS1, who presented slightly worse agreement.
CONCLUSIONSVisual estimation of the functional impact of intermediate coronary stenosis (40%-70%), even when taking into account factors other than the degree of stenosis, can lead to more than 30% disagreement with the results of invasive measurement of FFR using a cutoff of 0.80. Calcification, male sex, or lesions located in arteries perfusing large myocardial territories can lead to underestimating the functional significance of the lesion. The functional significance of lesions in vessels other than the left anterior descending artery, in-stent restenosis, and lesions in bifurcations tends to be overestimated by visual estimation. The invasive functional study of lesions with these characteristics is strongly indicated to avoid erroneous decisions to revascularize.
CONFLICTS OF INTERESTNone declared.