Keywords
INTRODUCTION
Epidemiology is the study of disease frequency and its determinants in the population.1 The term derives its meaning from the word epidemic, and in the first half of the last century the major epidemics were infectious disease outbreaks. With the discovery of antibiotics2 and the implementation of public health measures to control the spread of these diseases,3 mortality due to infections decreased and life expectancy increased. As a consequence of these changes a non-infectious group of diseases became the main individual cause of mortality: cardiovascular diseases. Around the middle of the last century cardiovascular disease mortality began to increase rapidly, but very little was known about its origins and causes.
Cardiovascular epidemiology began in the 1930's as a consequence of observed changes in the causes of mortality. In 1932, Wilhelm Raab described the relationship between diet and coronary heart disease (CHD) in different regions,4 and in 1953 an association between cholesterol levels and CHD mortality was reported in various populations.5
Several epidemiological studies were implemented in the 1950s to unravel the causes of cardiovascular disease (CVD).6-10 In 1948, the Framingham Heart Study was initiated by the USA Public Health Service to study the epidemiology and risk factors for CVD.11
That year, the National Institute of Health was expanded to encompass several institutes, each devoted to the study of particular diseases. The Framingham Heart Study was transferred to the National Heart Institute established in 1949, now known as the National Heart, Lung, and Blood Institute, and remains under its direction today. Since 1970 the Framingham Heart Study has also been closely affiliated with the Boston University. The town of Framingham, located 32 Km west of Boston, Massachusetts, was selected because it had been the site of a successful community-based tuberculosis study undertaken in 1918, and because of its proximity to Boston's major medical centers, the presence of several large employers and the support of a well-informed and highly cooperative medical and civil community.
The first cohort included 5209 healthy residents between 30 and 60 years of age enrolled in 1948 for biennial examinations which have continued since then. In 1971, 5124 sons and daughters (and their spouses) of the original cohort were recruited for the Offspring Study. Finally, in 2002, 4095 participants were included in the Third Generation cohort of the study.12 Some of the main findings and landmarks of the Framingham Heart Study are summarized in Figure 1.
Figure 1. Summary of some of the main findings and landmarks of the Framingham Heart Study. ADL-C indicates high density hipoprotein
In the 1950's, individuals who developed CVD were considered to be unlucky. By coining the expression "risk factor," the Framingham Heart Study helped to change the practice of medicine. Nowadays, we define a risk factor as a measurable element or characteristic that is causally associated with an increased rate of a disease and that is an independent and significant predictor of the risk of presenting a disease.
In this narrative review we will present some of the most relevant findings regarding the causes of CVD proceeding from the Framingham Heart Study, focusing on the identification of risk factors, the analysis of their predictive capacity, and the consequences of these findings for prevention.
THE JOURNEY TO IDENTIFY FACTORS ASSOCIATED WITH CARDIOVASCULAR DISEASE
Four years after the beginning of the Framingham Heart Study, with 34 cases of heart attack in the cohort, investigators identified high cholesterol and high blood pressure as important factors in the development of CVD.13 In the following years Framingham and other epidemiological studies contributed to the identification of other risk factors that are now considered to be classical risk factors for cardiovascular disease.
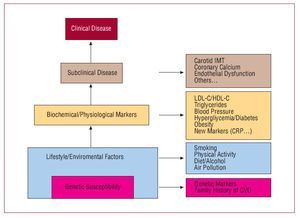
Cardiovascular risk factors can be classified in different ways. Figure 2 describes the relationship between the natural history of cardiovascular diseases and lifestyle and biochemical/physiological characteristics considered to be risk factors for these diseases, as well as subclinical disease markers.
Figure 2. Natural history of cardiovascular diseases and its correspondence with some lifestyle and biochemical/physiological characteristics considered risk factor for these diseases. CRP indicates C-reactive protein; CVD, cardiovascular disease; HDL-C, high density lipoprotein cholesterol; IMT, intimal medial thickness; LDL-C, low density lipoprotein cholesterol.
Lipids
When epidemiological studies began, there were some prior evidence that suggested a relationship between total cholesterol and atherosclerosis based on animal studies and clinical observations. This association was confirmed by epidemiological studies showing a strong relation between serum total cholesterol and cardiovascular risk10,14-16 and that changes in cholesterol levels due to migration17,18 or interventions19 where associated with changes in CVD incidence rate. In light of these studies, clinicians and epidemiologists agreed that total plasma cholesterol was a useful marker for predicting CVD. These findings were confirmed when low density lipoprotein cholesterol (LDL-C), the principal lipoprotein transporting cholesterol in the blood was also directly associated with CVD.20,21 Moreover, LDL cholesterol levels in young adulthood predict development of CVD later in life,22,23 supporting the idea that the relationship between LDL-C and development of CVD should be viewed as a continuous process beginning early in life. Current guidelines identify LDLC as the primary target for high blood cholesterol therapy.24 The efficacy of LDL-C lowering drug therapies to reduce CHD event rate and mortality has been shown in various clinical trials.24,25
Regarding LDL-C and considering the data from observational and experimental studies, it has been estimated that the benefits of reducing serum cholesterol for CHD risk are age-related. A 10% reduction in serum cholesterol produces a drop in CHD risk of 50% at age 40, 40% at age 50, 30% at age 60, and 20% at age 70.26
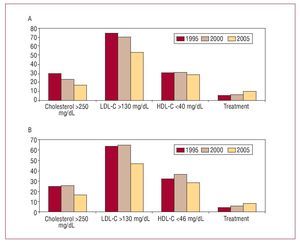
Figure 3. Trends in the proportion of the population of Girona with total, LDL and HDL cholesterol greater or lower than some cutpoints in the last 10 years. A indicates men; B, women. HDL-C indicates high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol.
Meanwhile, other studies were beginning to highlight the fact that individuals with high HDL levels were less likely to present CHD than individuals with low HDL levels.20,26 It was only after the publication of results from the Cooperative Lipoprotein Study27 and the Framingham Heart Study28 that HDL-C was accepted as an important factor related to atherosclerosis. Consequently, raising HDL cholesterol (HDL-C) levels has become an accepted therapeutic strategy for decreasing CHD incidence rate. Although there are some drugs, such as fibrates, niacin, and torcetrapib, a cholesteryl ester-transfer protein inhibitor, that have been shown to be effective in increasing HDL-C29,30 only fibrates have been shown to reduce risk of major coronary events; torcetrapib has in fact been shown to increase blood pressure and risk of mortality and morbidity through an unknown mechanism.31 It is estimated that a 1 mg/dL increase in HDL level is associated with a decrease in coronary risk of 2% in men and 3% in women.30
The role of triglycerides as an independent risk factor for CHD has been always controversial and, although some consistent evidence has been put forward, there are some doubts about the independent nature of this relationship.34
In Spain the prevalence of hypercholesterolemia is also high, and it is estimated that 23% of the adult population presents total cholesterol higher than 250 mg/dL.35 In Figure 3 we show the trends in the proportion of the population of Girona with total cholesterol, LDLC, and HDL-C greater or lower than various thresholds during the last 10 years.36
Hypertension
In 1948 it was thought that high blood pressure was necessary to force blood through the stiffened arteries of older persons and that it was a normal element of aging, therefore it was considered appropriate to ignore labile and systolic elevations of blood pressure37 and isolated systolic hypertension was rarely considered seriously.38
Framingham researchers dispelled these myths and reported that blood pressure was directly associated with cardiovascular risk regardless of how labile it was.39 Moreover, it was reported that isolated systolic hypertension was also a powerful predictor of cardiovascular disease.40
More importantly, Framingham and other epidemiological studies, demonstrated that systolic and diastolic blood pressure has a continuous, independent, graded, and positive association with cardiovascular outcomes.41-44 Even high-normal blood pressure values are associated with an increased risk of cardiovascular disease.45 In light of these studies, the Joint National Committee VII report developed a new classification of blood pressure for adults aged 18 years or older,46 including a new category called prehypertension, since these individuals are at increased risk of progression to hypertension and show an independent increased in risk of cardiovascular disease.
For individuals aged 40 to 70 years, each increment of 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic blood pressure doubles the risk of CVD across the entire range of blood pressure from 115/75 to 185/115 mm Hg.47 In clinical trials, antihypertensive therapy has been associated with a 35% to 40% reduction in stroke incidence; 20% to 25% in myocardial infarction; and more than 50% in heart failure.48
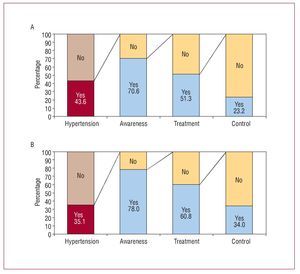
In Spain the prevalence of hypertension is high, and it is estimated to be around 34% in the adult population.35 In the population of Girona, the trends in awareness, treatment, and control have improved in the last 10 years although the proportion of controlled hypertension is still far from ideal (Figure 4).36
Figure 4.Trends in the prevalence, awareness, treatment, and control of hypertension in the population of Girona in the last 10 years. A indicates men; B, women.
Smoking
Before Framingham, smoking was not accepted as a bona fide cause of heart disease; even the American Heart Association issued a report en 1956 stating that the available evidence was insufficient to conclude that there was a causative relationship between cigarette smoking and CHD of incidence.49 The Framingham Study along with the Albany Cardiovascular Health Center Study soon demonstrated that smokers were at increased risk of myocardial infarction or sudden death.50 Moreover, risk was related to the number of cigarettes smoked each day, and former smokers had similar CHD morbidity and mortality to those who never smoked.50 These results were confirmed by other epidemiological studies,51-53 placing smoking as a high priority on the preventive agenda.
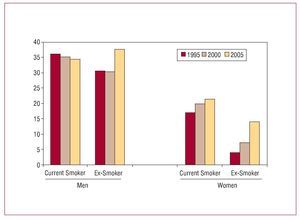
In Spain the prevalence of smoking is very high, and although it has decreased slightly in men, it has increased in women in the last decade (Figure 5).36
Figure 5. Trends in the prevalence of smoking in the population of Girona in the last 10 years.
Diabetes
Diabetes is associated with a 2- to 3-fold increase in the likelihood of developing CVD,54 this increase being higher in women than in men55; glucose intolerance is also associated with a 1.5-fold increase in the risk of developing cardiovascular disease.56
Moreover, diabetes is also associated with a higher probability of presenting with hypertrigliceridemia, low HDL-C, high blood pressure, and obesity, which usually precede the onset of diabetes.57 Insulin resistance has been suggested to be a common mechanism for these risk factors,58 the association of which is referred to as the metabolic syndrome,59 but there are still some doubts about the common mechanism and the added value of this diagnosis instead of the individual diagnosis of each component.60
In Spain, the prevalence of diabetes is 8% in women and 12% in men61 and seems to be stable, although the increase in the prevalence of obesity in this population may results in an increase in diabetes prevalence.62
Physical Inactivity
Since the first study of Morris et al published in 1953,63 a number of epidemiological studies have confirmed an association between physical inactivity and CHD.64 The relative risk of death from CHD for sedentary compared with active individuals is 1.9 (95% confidence interval 1.6-2.2).64 A recent study concluded that differences in known risk factors explain a large proportion (59.0%) of the inverse association between physical activity and CHD. Inflammatory/haemostatic biomarkers made the largest contribution to lower risk (32.6%), followed by blood pressure (27.1%), body mass index (10.1%), and hemoglobin A1c/diabetes (8.9%).65 The recommendation of physical exercise has become an important element of preventative policies in adults,66 elderly,67 and children.68
Obesity
Obesity is a chronic metabolic disorder associated with numerous comorbidities such as CHD,69 CVD,70 type 2 diabetes,62 hypertension,71 certain cancers, and sleep apnea. Obesity is also an independent risk factor for all-cause mortality,72,73 a relationship identified by Framingham investigators 40 years ago.74 In addition to alterations in metabolic profile, various adaptations in cardiac structure and function occur as excess adipose tissue accumulates.75 Similar to data observed with LDL-C and supporting the idea that the progression of atherosclerosis should be viewed as a continuous process beginning early in life, a recent study reported that higher BMI during childhood is associated with an increased risk of CHD in adulthood.76 This association seems to be stronger in boys than in girls and increases with the age of the child in both sexes.76
The prevention and control of overweight and obesity in adults and children has become a key element for the prevention of cardiovascular diseases.77-79
Novel Risk Factors
Although the misleading idea that the 4 major modifiable traditional cardiovascular risk factors —smoking, diabetes mellitus, hypertension, and hypercholesterolemia—account for "only 50%" of individuals who go on to develop CHD is widespread,80 major risk factor exposures are very common (>80%) among those who developed CHD81,82 and explain approximately 75% of the incidence of CHD,83 emphasizingthe importance of considering all major risk factors when estimating CHD risk and when attempting to prevent clinical CHD.
Nonetheless, research on non-traditional risk factors and genetic causes of heart disease is important to discovering new pathways related to atherosclerosis.84 In future articles of this series various authors will review specific aspects of these novel risk factors.
ASSESSMENT OF THE PREDICTIVE CAPACITY OF RISK FACTORS
Chronic diseases such as CVD are the result of complex interactions between genetic and environmental factors over extended periods of time. In this section we will analyze the ability of risk factors to predict future CVD events.
One of the contributions of Framingham investigators was to develop new multivariate statistical methods to analyze the development of complex disease.85 These methods allow us to estimate individual risk according to the level of exposure to different risk factors included in a mathematical function. Estimation of CHD and other cardiovascular events is a dynamic field and various functions have been proposed and developed by Framingham investigators.86-88 The most recent function was published in 1998 and develops a simplified coronary prediction model, using the blood pressure, cholesterol, and LDL-Ccategories proposed by the JNC-V and NCEP ATP II.88 One of the concerns related to the use of the Framingham risk function has been its generalizability to other communities, since it is based on the experience of the Framingham Study, a community sample of white subjects drawn from a suburb west of Boston. However, reasonable accuracy in predicting CHD has been demonstrated in various populations from the United States, Australia, and New Zealand, and although it overestimates the absolute risk in China and European populations,89 after recalibration for differing prevalences of risk factors and underlying rates of CHD events, it can be applied in different populations90 including the Spanish population.91,92
The accuracy of a risk function reflects on both the ability to distinguish individuals who will and will not develop the disease (discrimination), and the close matching of predicted and observed probabilities (calibration).
Discrimination is the ability of a prediction model to separate those who experience a CHD event from those who do not. It is usually quantified by calculating the c statistic, analogousto the area under a receiver operating characteristic (ROC) curve; this value is an estimate of the probabilitythat a model assigns a higher risk to those who develop CHDwithin a 5-year follow-up period than to those who do not.90
Calibration measures how closely predicted probabilities of CHD agree with actual outcomes. Calibration is evaluated by using a measure that summarizes how closely the predicted and observed risks agree within each decile of predicted risk (Hosmer-Lemeshow statistic). As mentioned above, when the risk function is used in populations with a probability of disease or a prevalence of risk factors that is very different from the population in which the risk function was developed, the function must be recalibrated to maintain its accuracy.90 At this point, it is important to note that although the incidence of CHD varies among populations, the relative risk associated with the level of exposure to the various risk factors is homogeneous across populations.93,94
The selection of risk factors to be included in a risk prediction equation is usually controversial, and involves the availability of methods to measure risk factors, the costs of those measurements, and general considerations of parsimony, and accuracy of the equation. Once the risk prediction equation is validated, however, the key question is how much the addition of a new risk factor improves prediction. The change in c-statistic, as a measure of the discrimination ability, provides one indication of that improvement.
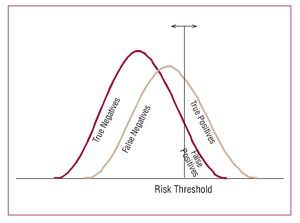
Although various new risk factors have been shown to be associated with CHD they have failed to significantly improve the discriminatory capacity of the classical Framingham risk function, even with a magnitude of association (measured as a odds ratio or hazard ratio) greater than 3.95,96 The reason for this failure can be explained by the overlap in the distributions of the risk factor between individuals with the disease and healthy individuals (Figure 6), which limits any improvement in the sensitivity and specificity of the predictive risk function.97 Similar difficulties in improving the discriminatory capacity of risk functions have been reported when using imaging techniques, such as carotid intima-media thickness or coronary calcium.98-100 More research remains to be done before new biomarkers can provide a basis for risk prediction at the individual level and to define the subset of individuals in which these biomarkers could add additional, complementary information.
Figure 6. Overlapping in the risk factor distribution between individuals with the disease and healthy individuals that explain the high proportion of false positive and negative individuals when using cardiovascular risk functions to predict cardiovascular events.
IMPLICATIONS FOR PREVENTION
At the time when the first results of epidemiological studies were emerging, opinions on the need to detect and treat asymptomatic risk factors, such as hypertension or hypercholesterolemia differed.101 However, the first results of the Framingham Heart Study revealed that much of the premature mortality due to CHD and stroke occurred in individuals generally prone to atherosclerosis, and in the context of identified risk factors presenting well in advance of the clinical symptoms.102 These observations resulted a paradigm change in perception of the causes of cardiovascular disease and encouraged physicians to place a greater emphasis on prevention, as well as on detecting and treating risk factors, and also to help individuals to understand that they could personally reduce their risk for heart disease. As Dr W. B. Kannel, a former chief investigator in the Framingham Heart Study, stated, "Cardiovascular events are coming to be regarded as a medical failure rather than the first indication of treatment."103 Sixty years after the beginning of the study, cardiovascular diseases remain the leading cause of global mortality and the morbidity related to these diseases is also high in Spain.104,105 However, some recent data indicates that incidence rates decreased in men aged 35-64 years during the period 1990-1999, but not in those aged 65-74 years, suggesting that preventative measures have increased the age at which a myocardial infarction or its recurrence is observed in men; no incidence rate changes were observed in women.106
Current guidelines provide advice on screening and identifying asymptomatic individuals at risk of developing CVD. The objectives of these guidelines are to reduce the incidence of first or recurrent clinical events due to coronary heart disease, ischemic stroke, and peripheral artery disease. The focus is on prevention of disability and early death. To thisend, the current guidelines address the role of lifestyle changes, the management of major cardiovascular risk factors and the use of different prophylactic drug therapies in the prevention of clinical CVD. The first step in this process is the calculation of individual cardiovascular risk according to risk factor exposure.24,107-110 Recent surveys indicate that guidelines awareness and acceptance is high, although implementation could be much improved.111-112 However, differences persist in the various guidelines regarding the methods of cardiovascular risk calculation, definitions of risk threshold, and definitions of who should be treated,113,114 causing confusion among clinicians, and this could be an important reason for failure in implementation of these guidelines in clinical practice.
On the other hand, we do not have to consider cardiovascular risk functions as diagnostic test because their sensitivity and specificity is low (Figure 6).114 These risk functions are screening test that help us to rationalize the selection of patients to implement different possible primary prevention strategies and their intensity.
Considering that cardiovascular diseases continue to be the leading cause of mortality in industrialized countries, more effort is required to reduce the burden of these diseases. In this context, lifestyle modifications based on avoiding smoking, taking regular physical exercise, and improving control of hypertension could be the most effective intervention at the population level. In Spain, it has been estimated that avoiding smoking and promoting physical activity could reduce the number or coronary heart disease deaths by 20% and 18% respectively115; controlling hypertension could reduce the number of cerebrovascular disease deaths by around 20%-25%.115