Bradyarrhythmias are a common clinical finding and comprise a number of rhythm disorders including sinus node dysfunction and atrioventricular conduction disturbances. Clinical presentation varies from asymptomatic electrocardiogram findings (eg, during a routine examination) to a wide range of symptoms such as heart failure symptoms, near syncope or syncope, central nervous symptoms, or nonspecific and chronic symptoms such as dizziness or fatigue. Conditions resulting in bradyarrhythmic disorders are divided into intrinsic and extrinsic conditions causing damage to the conduction system. Furthermore bradyarrhythmias can be a normal physiologic reaction under certain circumstances. A proper diagnosis including a symptom-rhythm correlation is extremely important and is generally established by noninvasive diagnostic studies (12-lead electrocardiogram, Holter electrocardiogram, exercise testing, event recorder, implantable loop recorder). Invasive electrophysiologic testing is rarely required. If reversible extrinsic causes of bradyarrhythmias such as drugs (most often beta-blockers, glycosides and/or calcium channel blockers) or underlying treatable diseases are ruled out, cardiac pacing is usually the therapy of choice in symptomatic bradyarrhythmias. In this article of the current series on arrhythmias we will review the pathophysiology, diagnosis and treatment options of bradyarrhythmias, especially sinus node dysfunction and atrioventricular conduction blocks.
Keywords
.
IntroductionBradyarrhythmias and conduction blocks are a common clinical finding and may be a physiologic reaction (for example in healthy, athletic persons) as well as a pathologic condition. Arbitrarily, bradyarrhythmias are defined as a heart rate below 60 beats per minute (bpm). These can be further categorized on the basis of the level of disturbances in the hierarchy of the normal cardiac conduction system.1The two major categories are sinus node dysfunction (SND) and atrioventricular (AV) conduction disturbances or blocks. In this article, we will review the pathophysiology, diagnosis, prognosis, and treatment options of these rhythm disorders. Further information can be obtained from the recently published book, Clinical Arrhythmology, by Antonio Bayes de Luna.2.
Clinical presentationClinical presentation of bradyarrhythmias varies from asymptomatic electrocardiographic findings to a broad array of symptoms which most bradycardias have in common (Table 1). Patients may present with near syncope and/or syncope, symptoms of heart failure such as dyspnea, angina, or premature mental incapacity, but also with nonspecific and chronic symptoms (dizziness, fatigue, lethargy). Symptoms can be either permanent or intermittent and unpredictable, as with SND..
Table 1. Symptoms of Bradyarrhythmias
| Dizziness, light-headedness, vertigo |
| Pre-syncope, syncope, Adam-Stokes attacks |
| Fatigue, lethargy |
| Angina, dyspnea |
| Congestive heart failure |
| Mental incapacity |
The physiologic conduction system consists of the sinus node, the AV node, and the bundle of His including the right and left bundle branch as well as the Purkinje system. The conduction system can be considered as a hierarchy of pacemakers with the sinus node being the primary pacemaker of the heart..
The sinus node was first identified as the region responsible for the primary activation of the heart by Keith and Flack in 1907.3 It is a crescent-shaped structure which lies epicardially in the sulcus terminalis between the superior vena cava and the right atrium. Although the sinus node is often depicted as a small, localized area in medical textbooks, this is not consistent with electrophysiologic findings.4, 5 According to experimental animal models (especially in rabbits), the sinus node is more likely to be a diffuse and extensive area between the superior and inferior vena cava.4, 6 It consists of spontaneously depolarizing pacemaker cells with a unique pattern of ion channels necessary for the generation and the propagation of action potentials. The sinus node is supplied with blood via the sinus node artery which originates from the right (about 60%) or the left (40%) circumflex coronary artery and approaches the sinus node from a clockwise or counterclockwise direction around the superior vena cava.1, 7, 8.
It has long been believed that impulses from the sinus node are conducted to the AV node via 3 intraatrial pathways (the anterior, middle and posterior internodal tract), but more recent studies suggest that atrial fiber orientation may account for preferred ways of conduction.1, 9, 10.
Apart from patients with accessory pathways the AV node is the sole connection between the atria and the ventricles. Impulses from the atria to the ventricle are modulated by the AV node. One of the main functions of the AV node is to delay and to limit the number of atrial impulses reaching the ventricle. Furthermore, the inferior nodal extensions of the AV node can act as a subsidiary pacemaker in cases of AV block.11 The AV node is part of the AV junction which can be divided into three different regions based on the marked heterogeneity in action potential waveform: the transitional zone, the compact portion or the AV node itself and the penetrating part of the AV bundle (His bundle).10, 11 The compact portion of the AV node is located beneath the right atrial endocardium, anterior to the coronary sinus ostium and above the insertion of the septal leaflet of the tricuspid valve.11 When entering the central fibrous tissue the AV node becomes the penetrating portion of the His bundle. Impulses are then conducted from the His bundle to the right and left bundle. The proximal part of the AV node is supplied by the AV nodal artery, whereas the distal part has a dual blood supply which makes it less vulnerable to ischemia.12 The AV nodal artery arises in 80% to 90% of humans from the right coronary artery and in 10% to 20% from the circumflex artery.1, 7, 12 Therefore, conduction abnormalities of the AV node during acute myocardial infarction are usually caused by an inferior myocardial infarction..
The cardiac conduction system is innervated by a rich supply of both, the sympathetic and parasympathetic nervous system. Stimulation of the sympathetic nervous system increases automaticity, enhances conduction, and shortens refractory periods. The parasympathetic influence has the opposite effect. The conduction in the His bundle, though, is neither influenced by sympathetic nor by vagal stimulation.10.
Sinus node dysfunctionSND (also called sick sinus syndrome in symptomatic patients) comprises a variety of disturbances affecting sinus node impulse generation and transmission within the atria and may lead to bradyarrhythmias but also tachycardias.13 It is sort of a spectrum of disorders. Possible electrocardiographic manifestations are:
• Persistent sinus bradycardia..
• Sinus pauses or arrest..
• Sinoatrial exit block..
• Chronotropic incompetence..
• Atrial tachycardia (including atrial fibrillation or atrial flutter), and thus,.
• Bradycardia-tachycardia syndrome..
Today, SND is still one of the major causes of pacemaker implantations other than AV block. It accounts for approximately 50% of pacemaker implantations in the United States, between 30% and 50% in Europe, and approximately 40% in Spain in 2009 and 2010.14, 15 In general, SND is a chronic progressive disorder and primarily occurs in the elderly with the incidence doubling between the fifth and sixth decades of life and the peak incidence in the seventh and eighth decades of life.16, 17 Although exact numbers on the incidence of SND are unavailable. SND is estimated to occur in 150 to 200 patients per million people.18.
Sinus BradycardiaBy convention, sinus bradycardia is defined by a heart rate below 60 bpm with the sinus node being the primary pacemaker. In the majority of cases sinus bradycardia is rather a physiologic reaction than a pathologic condition. Sinus bradycardia is a common, often transient finding and is predominantly caused by increased vagal tone. It is therefore seen in trained athletes and in healthy young adults at rest and at night (heart rate may fall below 30 bpm at night).19, 20, 21, 22 In patients with persistent sinus bradycardia, especially with documented heart rates slower than 40 bpm during daytime and symptoms of bradycardia, sinus bradycardia is pathologic and often a manifestation of SND.17, 18.
Sinus Pauses or ArrestSinus arrest or pauses imply failure of an expected atrial activation.23 This may be due to a problem of impulse generation in the sinus node or a failure of impulse conduction to the atrium. Though there are currently no cut-off values, pauses of 3s or more are uncommon and warrant implantation of a pacemaker in symptomatic patients.24, 25 Pauses of 3s or more, however, do not seem to be predictive of heightened mortality according to a newer study.26.
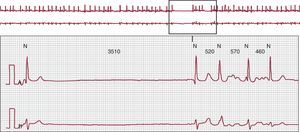
Pauses frequently occur in bradycardia-tachycardia syndrome (Figure 1) when an atrial tachyarrhythmia spontaneously terminates and sinus node recovery time is prolonged. This is the time during which no secondary or tertiary pacemaking center takes over until the sinus node resumes its activity. Reproducibility of such pauses by high-rate atrial pacing is relatively low. Suppression of sinus node activity may be aggravated by antiarrhythmic drugs..
Figure 1. An example of a patient with typical bradycardia-tachycardia syndrome: atrial fibrillation suddenly terminates and is followed by a pause until the first sinus beat due to a prolonged sinus node recovery time.
Chronotropic IncompetenceChronotropic incompetence is defined as the inability of the heart to adjust its rate adequately in response to increased physical activity or changing metabolic demands.23, 27 It is often missed in clinical practice, which may be in part due to missing universally accepted diagnostic criteria. The criterion used by the majority of physicians and studies is the failure to achieve 80% of the maximum predicted heart rate (220 minus age) at peak exercise during an exercise test.17, 23, 27.
Atrial tachyarrhythmias have been the subject of this series on arrhythmias and will therefore not be discussed here. The reader is referred to previous chapters addressing atrial tachycardia and atrial flutter28 and atrial fibrillation29..
Pathophysiology of Sinus Node DysfunctionSND can result from various conditions, which cause depression of the automaticity in and electrical conduction from the sinus node, perinodal and atrial tissue.16 These conditions may be intrinsic (diseases that directly alter the sinus node or sinoatrial structure) or extrinsic (most often cardiovascular drugs or systemic illnesses such as sleep apnea).23 Possible causes of SND are listed in Table 2. The most common cause of SND is idiopathic degenerative fibrosis of nodal tissue which is associated with aging.16, 30, 31 Fibrosis is thought to lead to a loss of pacemaker cells and a shift from central to inferior pacemaker cells within the sinus node.4, 32 Spontaneous diastolic depolarization is slower in those cells, which results in bradycardia..
Table 2. Causes of Sinus Node Dysfunction
| Extrinsic causes | Intrinsic causes |
| Pharmacologic agents* | Idiopathic degenerative fibrosis* |
| Betablockers | Ischemia (including infarction) |
| Calcium channel blockers | Infectious diseases |
| Cardiac glycosides | Chagas disease |
| Antiarrhythmic drugs (class I, III) | Endocarditis |
| Sympatholytic antihypertensives | Diphteria |
| Others: Lithium, Phenytoin | Inflammatory disease |
| Electrolyte disturbances | Myocarditis |
| Hypothyroidism | Infiltrative disorders |
| Sleep apnea | Collagen vascular diseases |
| Hypoxia | Musculoskeletal disorders |
| Hypothermia | Cardiothoracic surgery |
| Increased vagal tone | Valve replacement |
| Vomiting | Congenital heart disease |
| Coughing | |
| Defecation, micturition |
*Most common causes.
Although SND is (as mentioned above) often associated with underlying heart disease and is primarily a disease of the elderly, it is also known to occur in fetuses, infants, children, and young adults without obvious heart disease or other contributing factors.4, 33, 34 Furthermore familial cases consistent with autosomal dominant inheritance with reduced penetrance or recessive inheritance have been described.33, 35, 36, 37 In these patients with isolated or idiopathic SND, mutations have been identified in the gene for the cardiac sodium channel (SCN5A) and in the gene for HCN4 responsible for the funny current (If) in human nodal tissue.33, 38, 39, 40, 41.
Diagnosis of Sinus Node DysfunctionTo establish the diagnosis of SND it is crucial to find a causal relationship between the patients’ symptoms and the electrocardiogram (ECG) abnormalities mentioned above. Due to the predominantly intermittent and often unpredictable nature of SND this can be very difficult. Apart from a thorough medical history, a 12-lead surface ECG, Holter ECG recording (long-term ECG), and exercise testing are usually adequate. Whenever surface ECG and repetitive Holter recordings are incapable of documenting the cause of a patient‘s symptoms, an external event recorder or an implantable loop recorder should be considered. In patients with symptoms occurring more than once a month an external event recorder which can be kept for a maximum of 30 days is often sufficient. An implantable loop recorder may be used in patients with infrequent and transient symptoms in whom none of the aforementioned electrocardiographic recordings could achieve diagnostic information.1.
Invasive Electrophysiologic Study in Sinus Node DysfunctionElectrophysiologic studies are usually not required in patients with symptomatic bradyarrhythmias such as high grade or complete AV block or SND because the information given by the surface ECG is most often sufficient. However, electrophysiologic studies can be useful in patients with symptoms highly suspicious of AV conduction abnormalities or SND in whom a documentation on surface ECG or ambulatory Holter monitoring was not successful or in persistent, asymptomatic 2:1 AV block..
Treatment of sinus node dysfunctionTreatment should be restricted to those patients in whom a strong symptom-rhythm correlation has been documented.13, 42 Patients with asymptomatic SND do not require specific treatment. The first step is to rule out or treat reversible extrinsic causes of SND (Table 2) and to exclude physiologic sinus bradycardia. Pharmacologic therapy is not effective in SND..
If there are no reversible conditions causing SND, cardiac pacing should be implemented to relieve symptoms (Table 3). The mode of pacing has been a subject of numerous studies (Pacemaker Selection in the Elderly trial,43 Canadian Trial of Physiological Pacing,44 Mode Selection Trial in Sinus-Node Dysfunction45 Danish trial46). The endpoints of these studies, comparing atrial with ventricular based pacing, were mortality, atrial fibrillation, frequency of thromboembolic episodes including stroke, heart failure, pacemaker syndrome, and the patients’ quality of life.42 Based on these studies, pacing modes preserving AV synchrony (AAIR or DDDR) seem to be superior to ventricular pacing alone and are therefore recommended by current guidelines of the European Society of Cardiology (ESC).42 The results of the recently published study of the DANPACE Investigators47 challenge the notion that AAIR is the preferred mode and instead support the routine use of DDDR pacing instead of AAIR. However, AAIR is still recommended for certain patients with SND according to the ESC guidelines,42 but the AAIR mode was found to be associated with a higher incidence of atrial fibrillation and a 2-fold increased risk of pacemaker re-operations in the DANPACE study..
Table 3. Indications for Cardiac Pacing in Sinus Node Dysfunction According to the 2007 European Society of Cardiology Guidelines 42
| Clinical indication | Class | Level of evidence |
| 1. SND manifests as symptomatic bradycardia with/without bradycardia-dependent tachycardia. Symptom-rhythm correlation must have been established: spontaneously occurring, drug induced where alternative drug therapy is lacking | I | C |
| 2. Syncope with SND, either spontaneously occurring or at an electrophysiologic study | ||
| 3, SND manifests as symptomatic chronotropic incompetence | ||
| 1. Symptomatic SND, which is either spontaneous or induced by a drug for which there is no alternative, but no symptom-rhythm correlation has been documented. Heart rate at rest should be <40 bpm | IIa | C |
| 2. Syncope for which no other explanation can be made, but there are abnormal electrophysiologic findings (CSNRT>800 ms) | ||
| 1. Minimally symptomatic patients with SND, resting heart rate <40 bpm while awake and no evidence of chronotropic incompetence | IIb | C |
| 1. SND without symptoms including use of bradycardia-provoking drugs | III | C |
| 2. ECG findings of SND with symptoms no due directly or indirectly to bradycardia | ||
| 3. Symptomatic SND where symptoms can reliably be attributed to no essential medication |
CSNRT, corrected sinus node recovery time; ECG, electrocardiogram; SND, sinus node dysfunction.
Taking into account that atrial tachyarrhythmias, particularly atrial fibrillation, are common in patients with SND and thrombembolism is the most important cause of mortality in SND,23 oral anticoagulation should be considered in each patient with SND and a history of intermittent tachycardias. Oral anticoagulation should be implemented according to the latest ESC guidelines for the management of atrial fibrillation.48.
Prognosis of Sinus Node DysfunctionThe natural course of SND can be highly variable and is often unpredictable. However, patients with a history of syncope due to SND are likely to have recurrent syncope.49 Development of concomitant complete AV block is considered to be low with a median annual incidence of 0.6% (total prevalence of 2.1%) and so does not dominate the clinical course of SND.17 The incidence of sudden death seems to be low, too, and pacemaker therapy does not seem to improve overall survival, but improves morbidity.49, 50, 51, 52 Progression and prognosis of SND depend on several factors: age, coexistent cardiovascular diseases, concomitant AV conduction block, and atrial fibrillation resulting in a higher risk of thromboembolic complications.18, 53 In patients with SND and preserved left ventricular function who are treated with cardiac pacing, the pacing mode does not seem to influence the incidence of thromboembolic complications and survival.47But as mentioned above, atrial fibrillation seems to be more frequent in the AAIR mode..
Atrioventricular conduction blockAV conduction block is a disorder in which atrial impulses are conducted with a delay or are not at all conducted to the ventricles at a time when the AV conduction pathway is not physiologically refractory.1, 42 Historically, it was the first indication for cardiac pacing and still remains the major reason (approximately 50%) for pacemaker implantation.14, 15, 17 The incidence of AV conduction disturbances increases with age and is estimated to be up to 30% in selected groups.54, 55 Congenital AV block is rare and occurs in 1 in 15 000 to 1 in 22 000 live births.8, 55, 56, 57.
Based on ECG criteria, AV block is traditionally classified as first-, second-, or third-degree (complete) AV block. On the basis of intracardiac electrophysiological recordings, supra-, intra-, or infra-Hisian block can be differentiated..
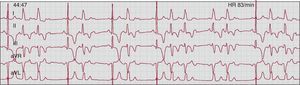
First Degree Atrioventricular BlockBy convention, first degree AV block is defined as an abnormal prolongation of the PR interval (>0.2s). Every P wave is followed by a QRS complex, but with a constantly prolonged PR interval. Prolongation of the PR interval can derive from delayed conduction within the atrium, AV node (AH interval) or His-Purkinje system (HV interval) but most commonly is due to delayed conduction within the AV node.58 Patients with first-degree AV block are usually asymptomatic. However, if a marked prolongation of the PR interval (>0.3s) occurs (Figure 2) patients may suffer from a pacemaker-like syndrome owing to AV dyssynchrony. Many of these patients are particularly symptomatic during exercise because the PR interval does not shorten appropriately as the R-R interval decreases.8.
Figure 2. An example of a patient with asymptomatic first-degree atrioventricular block with marked prolongation of the PR interval (PR 0.4 s). Every P wave is conducted with a constant PR interval. The amplitude of the P wave is higher than normal (0.3 mV-0.4 mV) and the P waves are diphasic in V1 (not shown on the electrocardiogram stripe) suggesting right atrial enlargement. Echocardiography and cardiac magnetic resonance imaging, however, were normal (calibration 25 mm/s, 10 mm/mV).
Second-Degree Atrioventricular BlockThe term second-degree AV block is applied when intermittent failure of AV conduction occurs.10 Second-degree AV block can be divided into 2 types based on ECG patterns: type I (Mobitz I or Wenckebach) and type II (Mobitz II). This classification should not be used to describe the anatomical site of the block because the terms type I and type II only refer to a certain ECG conduction pattern. To avoid mistakes and pitfalls often associated with the diagnosis of second-degree AV block, it is important to adhere to a correct definition.59.
The classic Mobitz type I second-degree AV block is characterized by a progressive PR interval prolongation prior to the nonconducted P wave (Wenckebach behavior). The first conducted P wave after the nonconducted P wave has the shortest PR interval of such a cycle and so the pause between the QRS complexes encompassing the nonconducted P wave will be less than twice the P-P interval.60 With stable sinus rhythm, the block cycle normally has a fixed P:R ratio (in classic type I ratios of 3:2, 4:3 or 5:4). However, many type I second-degree AV block sequences are atypical and do not show the classical progressive prolongation of the PR interval59, 61 (Figure 3)..
Figure 3. Atypical second-degree Mobitz type I (Wenckebach) atrioventricular block with a 6:5 ratio. The sequence in this patient does not follow the mathematical structure proposed by Wenckebach. The second to fourth PR intervals are prolonged but constant and it is the fifth, but not the second PR interval showing the greatest increment. The first conducted P wave after the nonconducted P wave has the shortest PR interval (240 ms). The pause between the QRS complexes encompassing the nonconducted P wave is less than two PP-intervals (calibration 25 mm/s, 10 mm/mV).
According to the statements of the World Health Organization and the American College of Cardiology a more appropriate definition of type I second-degree AV block is occurrence of a single nonconducted P wave associated with inconstant PR intervals before and after the blocked impulse as long as there are at least 2 consecutive conducted P waves (ie, 3:2 AV block) to determine the behavior of the PR intervals.62.
Type II second-degree AV block (Figure 4) is defined as the occurrence of a single nonconducted P wave associated with constant PR intervals before and after a single blocked impulse (PP and RR intervals are constant).58, 59 The pause encompassing the blocked P wave equals 2 P-P cycles. Type II second-degree AV block typically occurs in conjunction with intraventricular block..
Figure 4. Second-degree Mobitz type II atrioventricular block with intermittent left bundle branch block: the first three P waves (from left to right) are conducted with a constant PR interval of 140 ms; the fourth P wave is not conducted. The pause between the two QRS complexes encompassing the nonconducted P wave equals two PP intervals. The QRS complex of the first conducted P wave is narrow and recurs in a similar pattern. The following QRS complexes are wider (0.14 s) and fulfill the criteria of complete left bundle branch block. Mobitz type II pattern in the setting of left bundle branch block indicates block below the His bundle. HR, heart rate.
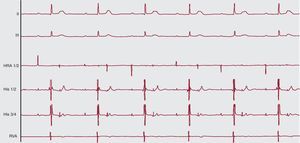
2:1 Atrioventricular BlockWith only one PR interval before the blocked P wave a 2:1 AV block (Figure 5), also called advanced AV block, cannot be classified as type I or II second-degree AV block based on a single (short) recording of the surface ECG. The anatomic site of the block can be in the AV node or in the His-Purkinje system and both type I or II second-degree AV block can progress or regress to a 2:1 block.59 The presence of intraventricular block indicates a block distal to the AV node, whereas a block with a small QRS complex is usually within the AV node. Considering that second-degree AV block type II is a class I indication for permanent pacing it is of huge therapeutic importance to make the exact diagnosis. Recording a long surface ECG strip, carotid sinus pressure test as well as giving atropine or exercise can reveal the correct type of second-degree AV block. If Wenckebach cycles are observed during long-term ECG recording (or sometimes during longer recordings of the standard ECG) of a patient with 2:1 AV block, this serves as an indication that in this case, 2:1 AV block most probably is the extreme form of a Wenckebach cycle..
Figure 5. A 15-year-old patient with second-degree atrioventricular block and intermittent third-degree atrioventricular block (not shown) during invasive electrophysiologic study (12-lead ECG, high right atrium, His and right ventricular apex catheter). The basic rhythm is a relatively stable sinus rhythm, but only every second P wave is conducted to the ventricle with a narrow QRS complex. The PR interval is constant (calibration 25 mm/s, 10 mm/mV). HRA, high right atrium; RVA, right ventricular apex catheter.
Third-Degree Atrioventricular BlockThird-degree or complete AV block is characterized by the failure of each P wave or each atrial impulse to conduct to the ventricle resulting in complete AV dissociation with atrial rates higher than the ventricular ones (Figure 6, Figure 7). It can be congenital or acquired and can be localized to the AV node, the His bundle, or the ramifications of the right and left bundles. The ventricular escape rhythm reveals the anatomic site of the block: complete AV block with an escape rhythm of 40 to 60 bpm and a narrow QRS complex on surface ECG is usually within the AV junction, which is often seen in congenital AV block (Figure 2). A wide QRS complex and/or a rate of 20 to 40 bpm imply a block in the His-Purkinje system, which is most often the case in acquired AV blocks.60.
Figure 6. An example of third-degree atrioventricular block with complete atrioventricular dissociation and an atrioventricular junctional escape rhythm with narrow QRS complexes (calibration 25 mm/s, 10 mm/mV).
Figure 7. Intermittent third-degree atrioventricular block with asystole in a patient who was admitted due to recurrent syncopes. The upper panel initially shows sudden onset of a third-degree atrioventricular block with no ventricular escape rhythm followed by an atrioventricular junctional escape rhythm with narrow QRS complexes in the lower panel (first 4 beats) as well as two conducted P waves at the end of the lower panel.
Etiology and Pathophysiology of Atrioventricular Conduction BlockAcquired AV block can be caused by a number of extrinsic and intrinsic conditions which were already discussed with SND (Table 2). Idiopathic progressive degeneration of the cardiac conduction system, referred to as Lenegre63 or Lev disease,64 accounts for approximately one half of cases of AV block. In addition to the causes listed under SND progressive AV conduction disturbances may be seen in neuromuscular disorders (muscular dystrophy, Kearns-Sayre syndrome), systemic diseases (eg, cardiac sarcoidosis, amyloidosis), neoplastic disorders (ie, primary cardiac lymphoma,65 and/or postradiation therapy), or after catheter ablation of septal accessory pathways or slow or fast AV pathway for AV nodal reentrant tachycardia. In younger individuals, Lyme disease should always be considered as a possible reversible cause of AV block..
Congenital complete AV block may occur as isolated disease which is frequently due to intrauterine exposure to maternal antibodies (Rho, La) or may be associated with any congenital heart disease.56, 57, 66 Pathologically, there are 4 types of congenital AV block: lack of connection between the atria and the peripheral conduction system, interruption of the AV bundle, bundle branch disease, and abnormal formation or interruption of the AV bundle.55 Complete AV block is a relatively frequent manifestation of the rare entity of congenitally corrected transposition of the great arteries..
Diagnosis of Atrioventricular BlockPatients presenting with advanced AV block generally complain of dizziness, vertigo and/or syncope, but may also suffer from any of the above mentioned symptoms of bradyarrhythmias. Diagnosis of AV block can be achieved in most of these cases noninvasively. The surface ECG (if the recording is sufficiently long) usually provides the information to characterize the type and localize the level of the block. In patients with intermittent AV block, Holter ECG and exercise testing are important to establish a correlation between symptoms and rhythm..
With rare exceptions such as persistent 2:1 AV block or failure to establish a symptom-rhythm correlation, invasive electrophysiologic study does not make a significant contribution to the management of patients with complete AV block..
Treatment of Atrioventricular Conduction BlocksAs with SND, treatment of AV block should start with looking for potentially reversible causes as for example Lyme disease or myocardial ischemia. Drugs resulting in a conduction delay within in AV node (eg, digitalis, calcium channel blockers) should be discontinued, if possible..
In the acute setting, symptomatic AV block can be treated with intravenous vagolytic agents as atropine and/or catecholamines (orciprenalin). If these drugs are not effective, a temporary pacemaker is indicated. In the emergency treatment of severe symptomatic bradyarrhythmias (no escape rhythm) transcutaneous stimulation may be applied..
Transient and permanent cardiac pacing is the definite therapy of choice in most cases of symptomatic complete AV block. The indication depends on the type and location of the AV block, present symptoms, the prognosis, and concomitant diseases. The exact recommendations of the ESC for cardiac pacing in acquired AV block are listed in Table 4..
Table 4. Recommendations for Cardiac Pacing in Acquired Atrioventricular Block According to the 2007 European Society of Cardiology Guidelines 42
| Clinical indication | Class | Level of evidence |
| 1. Chronic symptomatic third- or second-degree (Mobitz I or II) atrioventricular block | I | C |
| 1. Neuromuscular diseases (eg, myotonic muscular dystrophy, Kearns-Sayre syndrome, etc.) with third- or second-degree atrioventricular block | I | B |
| 3. Third- or second-degree (Mobitz I or II) atrioventricular block | I | C |
| • After catheter ablation of the atrioventricular junction | ||
| • After valve surgery when the block is not expected to resolve | ||
| 1. Asymptomatic third- or second-degree (Mobitz I or II) atrioventricular block | IIa | C |
| 2. Symptomatic prolonged first-degree atrioventricular block | IIa | C |
| 1. Neuromuscular diseases (eg, myotonic muscular dystrophy, Kearns-Sayre syndrome, etc.) with first-degree atrioventricular block | IIb | B |
| 1. Asymptomatic first-degree atrioventricular block | III | C |
| 2. Asymptomatic second-degree Mobitz I with supra-Hisian conduction block | ||
| 3. Atrioventricular block expected to resolve |
Patients with first-degree AV block usually do not need cardiac pacing. If the PR interval, though, fails to adapt to heart rate during exercise and is long enough (most often > 0.3 s) to cause symptoms due to loss of AV synchrony, implantation of a DDD pacemaker should be considered (class IIa).42.
Asymptomatic type I second-degree AV block (Wenckebach) is almost always considered a benign condition with excellent prognosis in young persons or well-trained athletes at rest.19, 20, 21, 22, 67 However, some controversy exists about the prognosis and the need for permanent pacing of chronic type I second-degree AV block in elderly patients (>45 years).8, 68, 69, 70 Thus, older patients with asymptomatic type I second-degree AV block should at least be monitored closely..
In patients with congenital complete AV block, the decision to implant a pacemaker is usually based on several factors including its natural history, the patient's age (significance of bradycardia is age-dependent) and symptoms, and the concomitant structural/congenital heart disease.42 The indications for permanent cardiac pacing in congenital complete AV block are still evolving. However, there is a consensus among pediatricians that the presence of an underlying severe heart disease, symptoms, and a heart rate below 50 to 55 bpm are an indication to implement cardiac pacing.42, 56 Nowadays, we also know that even asymptomatic patients with isolated congenital heart disease have an unpredictable risk of syncope, so that pacing should be strongly considered in each patient with congenital complete AV block.71, 72, 73.
Prognosis of Atrioventricular Conduction BlockThe prognosis of patients with AV conduction disturbances depends on the site of the block, but also particularly on the concomitant or underlying heart disease. The natural history of the different types of AV block dates back to the era before pacemaker therapy was available as there is no alternative therapy for patients with symptomatic AV block..
First-degree AV block carries an excellent prognosis because the risk of progression to third-degree AV block is extremely low.10, 74, 75 Controversy exists about the prognosis of chronic, type I second-degree AV block as mentioned above. In healthy young patients with normal QRS width, it is considered to be a benign condition.76 In older patients (>45 years) and in patients with associated bundle branch block suggesting an infranodal location prognosis seems to be worse compared with age- and sex-matched individuals unless a pacemaker is implanted.8, 68, 69.
The natural course of type II second-degree AV block is characterized by a high rate of progression to complete AV block. Patients have a significantly lower 5-year survival rate than patients who had a pacemaker implanted for second-degree AV block.68, 77.
In the absence of pacing, patients with acquired complete AV block have a very poor prognosis with 1-year survival rates only between 50% to 70% (compared to a sex- and age-matched control population) after having experienced syncope due to complete AV block.8, 42, 78, 79, 80, 81.
Prognosis of patients with congenital AV block is largely dependent on the presence of congenital heart disease and time of diagnosis.66 The prognosis of isolated congenital complete heart block is a more favorable one compared to those with concomitant structural heart disease.10, 81However, the stability of escape rhythms and the incidence of syncope are unpredictable. Cardiac pacing should be strongly considered even in asymptomatic patients with isolated congenital AV block.71, 72, 73 The occurrence of complex ventricular arrhythmias may also argue for pacemaker implantation in asymptomatic individuals..
Intraventricular conduction abnormalitiesIntraventricular conduction abnormalities including right bundle branch, left bundle branch, fascicular block, or a combination of these are commonly seen on routine ECG of elderly patients but may also been seen in younger patients either as an isolated finding or in association with dilative cardiomyopathy. The incidence was estimated to be 11% in men and 5% in women over 60 years according to an analysis of the Framingham study82 and is increasing with age..
Pathophysiology of Intraventricular Conduction AbnormalitiesIntraventricular conduction abnormalities and bundle branch blocks can be due to ischemia, ie, in myocardial infarction, after cardiothoracic surgery or can be mechanically induced after (mostly) aortic valve replacement surgery and after transcatheter aortic valve implantation. It can also be the consequence of surgery in congenital heart disease. Left bundle branch block (LBBB) that is defined by a prolongation of QRS above 0.11s in combination with a delay of the intrinsic deflection in leads V5 and V6 >60 ms (and no septal Q waves in leads I, V5 and V6) often occurs in association with dilative cardiomyopathy. However, the majority of chronic bundle branch block is idiopathic and seems to be associated with fibrosis of the conduction system, though only a few studies have investigated the underlying pathophysiology..
Prognosis of Intraventricular Conduction AbnormalitiesBundle branch block (especially LBBB) and bifascicular block are generally associated with a higher mortality compared to sex- and age-matched control persons, but some conditions such as isolated right bundle branch block are considered to be benign.42 The higher mortality is rather explained by the associated heart disease, especially coronary artery disease, than by the conduction abnormalities.83, 84, 85 However, LBBB itself may be a cause or an aggravating factor in left ventricular systolic failure due to the reduced pumping performance which results from asynchronous electrical activation of the ventricles in LBBB. In some cases a LBBB may be the first sign of a developing latent dilated cardiomyopathy.86.
The annual incidence of progression to advanced or complete AV block and so the risk of death from bradyarrhythmia is low.42, 87, 88, 89 Syncope and death seem to result more often from tachyarrhythmias and/or myocardial infarction than from conduction abnormality itself.87.
Diagnosis of Intraventricular Conduction AbnormalitiesThe ECG and the Holter ECG (in intermittent conduction delay) provide the information to identify the type of conduction delay. In patients with intraventricular conduction delays and a history of syncope invasive electrophysiologic study may be helpful. If the HV interval is more than 100ms, implantation of a pacemaker should be discussed.17, 42 According to the 2007 ESC guidelines an electrophysiologic study is also pathologic, if a high-degree His-Purkinje block is unmasked by intravenous administration of ajmaline.42 The relevance of ajmaline challenge in clinical practice, however, is not discussed..
Furthermore, every patient with bundle branch block should be evaluated for an underlying structural heart disease due to the high incidence of coronary artery and/or hypertensive heart disease. In general, the incidence is higher with left bundle branch than with right bundle branch..
Therapy of Intraventricular Conduction AbnormalitiesBecause of the low incidence of complete AV block, asymptomatic patients with isolated right or left or bifascicular block with or without first-degree AV block (often wrongly referred to as “trifascicular” block) do not require permanent cardiac pacing. According to the ESC guidelines, a cardiac pacemaker should be implanted in patients with true trifascicular block (ie, alternating bundle branch block), chronic bifascicular block, and second-degree Mobitz II AV block, or intermittent complete AV block. The detailed recommendations are summarized in Table 5..
Table 5. Recommendations for Cardiac Pacing in Chronic Bifascicular and Trifascicular Block According to the 2007 European Society of Cardiology Guidelines 42
| Clinical indication | Class | Level of evidence |
| 1. Intermittent third-degree atrioventricular block | I | C |
| 2. Second-degree Mobitz II atrioventricular block | ||
| 3. Alternating bundle branch | ||
| 4. Findings on electrophysiological study of markedly prolonged HV interval (≥100 ms) or pacing-induced infra-His block in patients with symptoms | ||
| 1. Syncope not demonstrated to be due to atrioventricular block when other likely causes have been excluded, specifically ventricular tachycardia | IIa | B |
| 2. Neuromuscular diseases (eg, myotonic muscular dystrophy, Kearns-Sayre syndrome, etc.) with any degree of fascicular block | IIa | C |
| 3. Incidental findings on electrophysiological study of markedly prolonged HV interval (≥100 ms) or pacing-induced infra-His block in patients without symptoms | IIa | C |
| 1. Bundle branch block without atrioventricular block or symptoms | III | B |
| 2. Bundle branch block with first-degree atrioventricular block without symptoms |
Apart from bradyarrhythmias patients with LBBB and dilative cardiomyopathy should be evaluated for cardiac resynchronization therapy..
Bradyarrhythmias associated with acute myocardial infarctionBradyarrhythmias arising in the setting of acute myocardial infarction are common and result from abnormalities in impulse formation or impulse conduction.90 Sinus bradycardia is one of the most common rhythm disorders related to myocardial infarction, especially in right coronary involvement (about 30%-40%).91.92 The major conduction abnormalities associated with myocardial infarction are AV and intraventricular conduction disorders.42 Despite new techniques such as thrombolysis and percutaneous coronary intervention the incidence of intraventricular conduction disturbances has not changed significantly; the absolute incidence of AV block, however, has decreased but remains still high.42, 93, 94, 95, 96, 97 AV block occurs in 6% to 7%93 of cases of acute myocardial infarction and is 2 to 3 times as commonly associated with inferior than anterior infarction.94, 95, 98 Intraventricular conduction delays occur in a transient form in up to 18% of patients and in approximately 5% in a persistent form.42, 99.
Pathophysiology of Bradyarrhythmias Associated With Acute Myocardial InfarctionThe pathophysiologic mechanisms underlying most bradyarrhythmias in myocardial infarction are: reversible ischemia, irreversible necrosis of the conduction system, or other conditions like altered autonomic function, such as increased parasympathetic tone, electrolyte disturbances, systemic hypoxia, or local increases in adenosine.90, 94, 100 According to histologic studies, obvious structural damage to the conduction system (necrosis) seems to be rare and is usually due to an extensive anterior myocardial infarction with necrosis of the septum.101, 102.
Treatment of Bradyarrhythmias Associated With Acute Myocardial InfarctionAcute management of symptomatic high-grade AV block includes intravenous drugs such as atropine or temporary cardiac pacing. Implantation of a permanent cardiac pacemaker is rarely necessary in acute myocardial infarction, especially in inferior myocardial infarction because truly persistent AV block is uncommon.94, 103 Recommendations for permanent cardiac pacing according to the ESC are:42
1. Persistent third-degree heart block preceded or not by intraventricular conduction disturbances..
2. Persistent Mobitz type II second-degree heart block associated with bundle branch block, with or without PR prolongation..
3. Transient Mobitz type II second- or third-degree heart block associated with new onset bundle branch block..
The huge problem with the recommendations for cardiac pacing in acute myocardial infarction is the definition of “persistent”. According to the ESC guidelines42 conduction disturbances are persistent if they do not resolve after more than 14 days. However, this has been and still is a subject of discussion..
Prognosis of Bradyarrhythmias Associated With Acute Myocardial InfarctionDespite the use of thrombolytic therapy and of percutaneous coronary intervention, AV block, and intraventricular conduction disturbances complicating acute myocardial infarction are still associated with a high risk of short-term, especially 30-day, mortality.42, 93, 94, 97, 98.
Conflicts of interestNone declared..
Received 16 January 2012
Accepted 20 January 2012
Corresponding author: Abteilung für Rhythmologie, Department für Kardiologie und Angiologie, Universitätsklinikum Münster, Albert-Schweitzer-Campus 1, 48149 Münster, Germany. Julia.Vogler@ukmuenster.de