Aortic intramural hematoma (AIH) is considered a precursor of aortic dissection. It is caused by vasa vasorum bleeding in the tunica media of the aortic wall. The incidence of AIH ranges from 3% to 53% of cases of acute aortic syndrome. The condition usually manifests as retrosternal pain with interscapular irradiation. It can progress to rupture or calcification, or it can regress. Aortic intramural hematoma is diagnosed by computed tomography (CT), magnetic resonance or transesophageal ultrasonography. The treatment is similar to that used in aortic dissection.
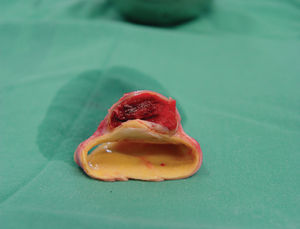
The case presented is a 62-year-old patient in whom a 4x3.5x2.5-cm soft, bluish mass was unexpectedly discovered in the distal portion of the ascending aorta (AA) during coronary surgery. The adventitia presented a moderate inflammatory reaction with minor pericardial adhesions. The AA measured 4.5 cm in diameter in this area (Figure 1). A decision was made during surgery to replace the AA with a 30-mm dacron graft. Upon opening the surgical specimen, examination of the AIH showed integrity of the intima without continuity with the aortic lumen (Figure 2). The hematoma had a soft consistency and contained an organized reddish thrombus, probably a consequence of recent bleeding from the vasa vasorum (Figure 3). The patient had experienced atypical anginal pain 8 days before surgery. The chest CT at discharge showed good surgical reconstruction of the AA, signs of moderate atheromatosis of the aortic arch, and no important changes in the descending thoracic aorta.
Figure 1.
Figure 2.
Figure 3.