To examine the extent to which the decrease in mortality rates in Spain between 1988 and 2005 could be explained by changes in cardiovascular risk factors and by the use of medical and surgical treatments.
MethodsWe used the previously validated IMPACT model to examine the contributions of exposure factors (risk factors and treatments) to the main outcome, changes in the mortality rates of death from coronary heart disease, among adults 35 to 74 years of age. Main data sources included official mortality statistics, results of longitudinal studies, national surveys, randomized controlled trials, and meta-analyses. The difference between observed and expected coronary heart disease deaths in 2005 was then partitioned between treatments and risk factors.
ResultsFrom 1988 to 2005, the age-adjusted coronary heart disease mortality rates fell by almost 40%, resulting in 8530 fewer coronary heart disease deaths in 2005. Approximately 47% of the fall in deaths was attributed to treatments. The major treatment contributions came from initial therapy for acute coronary syndromes (11%), secondary prevention (10%), and heart failure (9%).
About 50% of the fall in mortality was attributed to changes in risk factors. The largest mortality benefit came from changes in total cholesterol (about 31% of the mortality fall) and in systolic blood pressure (about 15%). However, some substantial gender differences were observed in risk factor trends with an increase in diabetes and obesity in men and an increase in smoking in young women. These generated additional deaths.
ConclusionsApproximately half of the coronary heart disease mortality fall in Spain was attributable to reductions in major risk factors, and half to evidence-based therapies. These results increase understanding of past trends and will help to inform planning for future prevention and treatment strategies in low-risk populations.
Keywords
.
INTRODUCTIONCoronary heart disease (CHD) incidence and mortality rates in southern Europe have been consistently three-fold lower than those observed in the rest of Europe or the United States, in spite of similar levels of cardiovascular risk factors. This reflects the so-called “Mediterranean Paradox”.1, 2 Furthermore, age-adjusted CHD death rates in people aged 35 to 74 have steeply decreased in Spain, by 40% since about 1980.3
This mortality decline could be explained in terms of risk factor trends or the use of evidence-based treatments, or a combination. For example, in Spain there were important recent improvements in cholesterol levels, hypertension treatments, and blood pressure control.4 The widespread use of effective evidence-based treatments has also improved, with decreases in acute myocardial infarction (AMI) 28-day case fatality observed since the 1990s.5
However, quantifying the relative contributions of these two contrasting components is a complex task. The use of epidemiological models is therefore becoming an increasingly important tool to address these difficult questions, by integrating data on risk factor trends and treatment effectiveness.6
Our objective was therefore to examine trends from CHD deaths in Spain between 1988 and 2005 by using IMPACT, a comprehensive CHD policy model now validated in over a dozen countries.6, 7, 8, 9, 10, 11
METHODSTo examine the contributions of various factors to the changes in mortality rates of death from CHD among Spanish adults aged 35 to 74 years, we used an updated version of the IMPACT policy model. This model has been previously validated in diverse populations of other countries in Europe, the United States, New Zealand, China,6, 7, 8, 9, 11 and–crucially–in another “Mediterranean” population, Italy.12
The IMPACT model methodology has been described in detail elsewhere.6 In brief, it is comprehensive, incorporating the major population risk factors for CHD (smoking, high blood pressure, elevated total cholesterol, obesity, diabetes, and physical inactivity) and all the usual medical and surgical treatments for CHD.
Wherever possible, data sources specific to the Spanish population were used to construct the Spanish IMPACT model (Table 1). When more than one data source was available, we selected the most recent, representative, and least biased source.
Table 1. Main Data Sources for the Parameters Used in the Spanish IMPACT Model for 1988 and 2005.
| 1988 | 2005 | |
| Population, deaths, CHD Mortality | National Statistics Institute | National Statistics Institute |
| Number of patients admitted yearly: MI, AP, HF | Hospital Morbidity Survey | Hospital Morbidity Survey |
| Number of CABG patients | Assume zero | Revista Española de Cardiología |
| PTCA | Assume zero | |
| Cardiopulmonary resuscitation in the community | IBERICA, REGICOR | IBERICA, REGICOR |
| AMI | Assume zero | REGICOR, MASCARA |
| Unstable angina pectoris | Assume zero | MASCARA, EMMA Researchers personal communication |
| Secondary prevention following AMI | Assume zero | REGICOR, EMMA Researchers personal communication |
| Secondary prevention following CABG or PTCA | Assume zero | REGICOR, EMMA Researchers personal communication |
| Congestive heart failure | Assume zero | EPISERVE Study; The PRICE Study |
| Treatment for chronic angina | Assume zero | REGICOR |
| Community angina pectoris: total | PANES | EMMA Researchers personal communication |
| Community chronic heart failure | ||
| Prevalence | Literature review | EMMA Researchers personal communication |
| Medication (ACE inhibitors, beta blockers, spironolactone, acetylsalicylic acid, statins) | Assume zero | EMMA Researchers personal communication |
| Hypertension | Banegas24 | REGICOR |
| Statins for primary-prevention | HERMES | |
| Population risk factor prevalence | ||
| Current smoking | National Health Survey | National Health Survey |
| Systolic blood pressure | CINDI Study | Baena Díez et al 37 |
| Cholesterol | MONICA-Cat | HERMES |
| Physical activity | National Health Survey | National Health Survey |
| Obesity (BMI) | MONICA-Cat | REGICOR |
| Diabetes | National Health Survey | National Health Survey |
ACE, angiotensin-converting enzyme; AMI, acute myocardial infarction; AP, angina pectoris; BMI, body mass index; CABG, coronary artery bypass grafts surgery; CHD, coronary heart disease; HF, heart failure; MI, myocardial infarction; PTCA, percutaneous transluminal coronary angioplasty.
Data for 1988 and 2005 on the total Spanish population and age distribution, and on deaths associated with CHD, all stratified by age and sex, were obtained from the Spanish Statistical Office.3 We then used internal standardization to estimate the number of CHD deaths that would have been expected in 2005 if the mortality rates in 1988 had remained unchanged. The age-specific mortality rates for 1988 were multiplied by the population for each 10-year age stratum in 2005 (thus accounting for population aging and growth). Three-year averages were employed to further reduce random variation.
Subtracting the number of deaths actually observed in 2005 from the number expected yielded the fall in the number of deaths in 2005 compared with the 1988 baseline that the model would have to explain.
Treatment and Mortality ReductionsThe number of patients with CHD categorized by diagnosis was obtained from the Spanish Hospital Morbidity Survey.3 The estimated frequency of use of specific treatments, the case fatality rate, and the risk reduction due to treatment, all stratified by age and sex, were obtained from published sources (Supplementary material).
The number of deaths prevented or postponed as a result of each intervention in each group of patients in 2005, stratified by age, was then calculated. The number of people in each diagnostic group of patients in 2005 was multiplied by the proportion of those patients who received a particular treatment, by their case fatality rate over a period of 1 year, and by the relative reduction in the 1-year case fatality rate reported for that treatment in the largest and most recent meta-analysis.6
For example, about 10 752 men aged 55 to 64 years were hospitalized with AMI in Spain in 2005. The expected age-specific 1-year case-fatality rate was approximately 5.4%. Approximately 79% were prescribed acetylsalicylic acid,13 with an expected mortality reduction of 15%. The number of deaths prevented or postponed for at least a year by the use of acetylsalicylic acid among men aged 55-64 were then calculated as:
To address the potential effect on the relative reduction in the case fatality rate for individual patients receiving multiple treatments, we used the Mant and Hicks cumulative-relative-benefit approach14:
We assumed that adherence, or the proportion of treated patients actually taking therapeutically effective levels of medication, was 100% among hospitalized patients, 70% among symptomatic patients in the community, and 50% among asymptomatic patients in the community.15, 16 To avoid double counting of patients treated, we identified potential overlaps between different groups of patients and made appropriate adjustments.
Risk Factors and Mortality ReductionsTwo approaches were used to calculate the number of deaths prevented or postponed as a result of changes in specific risk factors.
We used a regression approach for systolic blood pressure, total cholesterol, and body mass index. The number of deaths prevented or postponed as a result of the change in the mean value for each of these risk factors was estimated as the product of 3 variables: the number of deaths from CHD in 1988 (the base year), the subsequent reduction in that risk factor, and the regression coefficient quantifying the change in mortality from CHD per unit of absolute change in the risk factor (obtained from a large, recent meta-analysis).
For example, in 1988, there were 3028 CHD deaths among 2 035 451 men aged 55-64 years. Mean systolic blood pressure in this group decreased by 2.4mmHg between 1988 and 2005. The largest metaanalysis reports an estimated age- and sex-specific reduction in mortality of 2.5% for every 1mmHg reduction in systolic blood pressure, thereby generating a logarithmic coefficient of –0.035.17
The population-attributable risk fraction approach was used to determine the effect of changes in the prevalence of smoking, diabetes, and physical inactivity.18 This is detailed in the Supplementary material.
The number of deaths prevented or postponed as a result of changes in risk factors was systematically quantified for each specific patient group to account for potential differences in effect.
We assumed that lag times between the change in the risk factor rate and the change in the event rate would be relatively unimportant over a period of 17 years.
Because independent regression coefficients and relative risks for each risk factor were obtained from multivariate analyses, we assumed that there was no further synergy between the treatment and risk-factor sections of the model or among the major risk factors.
Comparison of Estimated and Observed Mortality ChangesThe model estimates for the total number of deaths prevented or postponed by each risk-factor change were then summed and compared with the observed changes in mortality for men and women in each age group. Any shortfall in the overall model estimate was then presumed to be attributable either to inaccuracies in our calculations or to other unmeasured risk factors. All estimates were rounded to the nearest multiple.
Sensitivity AnalysisWe tested all the above assumptions and variables in a multiple-way sensitivity analysis, using the analysis-of-extremes method.19 For each variable in the model, we assigned a lower value and an upper value, using 95% confidence intervals when available and otherwise using ±20% (for the number of patients, treatment use, and compliance).13, 20
Detailed information on methods and data sources is shown in the Supplementary material.
RESULTSFrom 1988 to 2005, the age-adjusted mortality rate of CHD fell from 148.2 to 92.1 cases per 100 000 population among men aged 35 to 74 years and from 46.7 to 24.2 among women aged 35 to 74 years. This resulted in 8530 fewer deaths in 2005 compared with the expected number if the rates in 1988 had persisted (20 610 expected minus 12 080 observed).
The Spain IMPACT model explained approximately 8310 (97%) of this 8530 decrease. Under the assumptions of the sensitivity analysis, the extreme minimum and the maximum number of deaths from CHD that were explained was 5045 (59%) and 13 830 (162%).
Medical and Surgical TreatmentsApproximately 3990 (47%) fewer CHD deaths were attributable to medical therapies (minimum estimate 1650, maximum estimate 8625) (Table 2). The largest mortality reductions came from the use of secondary prevention medications (after post-myocardial infarction or after percutaneous transluminal coronary angioplasty/coronary artery bypass grafts surgery, approximately 855 fewer deaths) and initial treatments for AMI or unstable angina (approximately 975 deaths), followed by the treatments of heart failure and hypertension, statins for primary prevention, and medical treatments for chronic angina. Revascularization for chronic angina resulted in approximately 170 fewer deaths in 2005 compared with 1988, or approximately 2% of the total mortality fall (Table 2).
Table 2. Estimated Attributable Effect of Treatments on the 8530 Coronary Heart Disease Deaths Prevented or Postponed in Spain in 2005.
| Patients elegible | Treatment uptake (%) | Relative risk reduction | Mean case-fatality | Deaths Prevented or Postponed | ||||
| Best estimate | Minimum estimate | Maximum estimate | % of total | |||||
| Acute phase disease management | ||||||||
| Acute myocardial infarction | ||||||||
| Community CPR | 13 672 | 3 | 0.08 | 0.066 | 20 | 16 | 55 | 0.3 |
| Hospital CPR | 892 | 100 | 0.33 | 0.066 | 275 | 69 | 375 | 3.2 |
| Thrombolysis | 44 617 | 30 | 0.27 | 0.066 | 205 | 163 | 245 | 2.4 |
| Acetylsalicylic acid | 44 617 | 78 | 0.15 | 0.066 | 215 | 171 | 620 | 2.5 |
| Primary PTCA | 44 617 | 3 | 0.28 | 0.066 | 25 | 17 | 57 | 0.3 |
| Beta blocker | 44 617 | 20 | 0.04 | 0.066 | 40 | –30 | 125 | 0.5 |
| ACE inhibitor | 44 617 | 13 | 0.07 | 0.066 | 40 | 5 | 59 | 0.5 |
| Primary CABG | 44 617 | 1 | 0.39 | 0.066 | 10 | 5 | 16 | 0.1 |
| Treatment effect already existing in 1988 | --- | --- | --- | --- | –170 | –38 | –225 | –2.0 |
| Total AMI | 44 617 | --- | --- | 0.066 | 660 | 378 | 1327 | 7.7 |
| Unstable angina | ||||||||
| Acetylsalicylic acid and Heparin | --- | 67 | 0.33 | 0.184 | 195 | 62 | 208 | 2.3 |
| Acetylsalicylic acid alone | --- | 20 | 0.15 | 0.184 | 15 | 8 | 28 | 0.2 |
| GP IIB/IIA | --- | 18 | 0.09 | 0.184 | 10 | 5 | 16 | 0.1 |
| Primary CABG | --- | 20 | 0.43 | 0.184 | 50 | 24 | 81 | 0.6 |
| Primary PTCA | --- | 30 | 0.28 | 0.184 | 45 | 24 | 79 | 0.5 |
| Total unstable angina | 14 151 | --- | --- | 0.184 | 315 | 123 | 412 | 3.7 |
| Total AMI+ unstable angina | --- | --- | --- | --- | 975 | 501 | 1739 | 11.4 |
| Secondary prevention | ||||||||
| Myocardial infarction | ||||||||
| Acetylsalicylic acid | --- | 74 | 0.15 | 0.037 | 160 | 65 | 327 | 1.8 |
| Beta blocker | --- | 41 | 0.23 | 0.037 | 170 | 72 | 365 | 2.1 |
| ACE inhibitor | --- | 42 | 0.20 | 0.037 | 145 | 60 | 301 | 1.7 |
| Statin | --- | 64 | 0.22 | 0.037 | 165 | 67 | 341 | 1.9 |
| Warfarin | --- | 6 | 0.22 | 0.037 | 35 | 11 | 58 | 0.4 |
| Rehabilitation | --- | 7 | 0.26 | 0.037 | 5 | 3 | 16 | 0.1 |
| Treatment effect already existing in 1988 | –10 | –5 | –20 | |||||
| Total myocardial infarction | 268 545 | --- | --- | 0.037 | 670 | 280 | 1405 | 7.9 |
| Post-CABG surgery/PTCA | ||||||||
| Acetylsalicylic acid | --- | 80 | 0.15 | 0.015 | 45 | 19 | 97 | 0.5 |
| Beta blocker | --- | 44 | 0.23 | 0.015 | 35 | 15 | 75 | 0.4 |
| ACE inhibitor | --- | 42 | 0.20 | 0.015 | 30 | 12 | 62 | 0.3 |
| Statin | --- | 63 | 0.22 | 0.015 | 50 | 20 | 102 | 0.6 |
| Warfarin | --- | 6 | 0.22 | 0.015 | 5 | 2 | 11 | 0.1 |
| Rehabilitation | --- | 3 | 0.26 | 0.015 | 5 | 1 | 6 | 0.1 |
| Total post-CABG surgery/PTCA | 66 808 | --- | --- | --- | 170 | 69 | 353 | 2.0 |
| Total AMI+total post-CABG surgery/PTCA | 855 | 347 | 1761 | 10.0 | ||||
| Chronic angina | ||||||||
| CABG surgery 1995-2005, minus 1988 | 65 054 | 100 | 0.15 | 0.016 | 170 | 155 | 806 | 2.0 |
| Angioplasty 1995-2005 | 0 | 100 | 0.13 | 0.003 | 0 | 0 | 0 | 0 |
| Acetylsalicylic acid in community | 441 255 | 78 | 0.15 | 0.0103 | 200 | 82 | 414 | 2.3 |
| Statins in community | 441 255 | 69 | 0.23 | 0.0103 | 200 | 82 | 417 | 2.3 |
| Total chronic angina | 441 255 | --- | --- | --- | 570 | 319 | 1637 | 6.7 |
| Heart failure (hospital management) | ||||||||
| ACE inhibitor | --- | 48 | 0.20 | 0.213 | 120 | 52 | 261 | 1.4 |
| Beta blocker | --- | 28 | 0.35 | 0.213 | 125 | 53 | 267 | 1.5 |
| Spironolactone | --- | 6 | 0.30 | 0.213 | 25 | 10 | 50 | 0.3 |
| Acetylsalicylic acid | --- | 38 | 0.15 | 0.213 | 60 | 31 | 155 | 0.7 |
| Total heart failure (hospital management) | 9735 | --- | --- | --- | 330 | 146 | 733 | 3.9 |
| Heart failure (community management) | ||||||||
| ACE inhibitor | --- | 30 | 0.20 | 0.078 | 95 | 37 | 233 | 1.1 |
| Beta blocker | --- | 27 | 0.35 | 0.078 | 225 | 91 | 463 | 2.6 |
| Spironolactone | --- | 4 | 0.36 | 0.078 | 25 | 10 | 52 | 0.3 |
| Acetylsalicylic acid | --- | 23 | 0.15 | 0.078 | 85 | 48 | 243 | 1.0 |
| Total heart failure (community management) | 65 715 | --- | --- | --- | 430 | 186 | 991 | 5.0 |
| Primary prevention | ||||||||
| Hypertension treatments | 7 735 137 | 43 | 0.13 | 0.002 | 775 | 125 | 1625 | 9.1 |
| Statins for primary prevention | 12 985 919 | 9 | 0.24 | 0.001 | 70 | 28 | 141 | 0.8 |
| Total primary prevention | --- | --- | --- | --- | (845) | 153 | 1764 | 9.9 |
| Total treatments | --- | --- | --- | --- | 3990 | 1650 | 8625 | 46.8 |
ACE, angiotensin-converting enzyme; AMI, acute myocardial infarction; CABG, coronary artery bypass grafts surgery; CPR, cardiopulmonary resuscitations; GP, glycoprotein; PTCA, percutaneous transluminal coronary angioplasty (with or without stent).
Numbers of eligible patients and category totals of deaths prevented or postponed were rounded to nearest 0 or 5; totals may therefore not always be exact.
Additional details of data sources are described in the Supplementary material .
Approximately 4320 fewer CHD deaths were attributable to changes in risk factors (minimum estimate 3395, maximum estimate 5205, Table 3). Decreases in total cholesterol concentration (–0.3 mmol/L), systolic blood pressure (–3.3mmHg), and smoking prevalence (–3.9%), were estimated to have prevented or postponed approximately 3130, 2045, and 1385 deaths, respectively. The 7.7% decrease in physical inactivity prevented or postponed approximately 195 deaths. In contrast, the 0.4kg/m2 increase in body mass index and 0.6% increase in diabetes prevalence resulted overall in approximately 535 and 640 additional deaths, respectively (Table 3).
Table 3. Estimated Attributable Effect of Risk Factor changes on the 8530 Coronary Heart Disease Deaths Prevented or Postponed in Spain from 1988 to 2005.
| Risk Factor | Absolute level of risk factor | Absolute risk factor change | Regression coefficient | Deaths prevented or postponed | ||||
| 1988 | 2005 | Best estimate | Minimum | Maximum | % of total a | |||
| Systolic blood pressure (mmHg) | ||||||||
| Men | 133.8 | 130.2 | –3.6 | –0.033 | 1165 | 757 | 1644 | 13.6 |
| Women | 128.1 | 124.9 | –3.2 | –0.04 | 880 | 578 | 1221 | 10.2 |
| Both sexes | 130.8 | 127.5 | –3.3 | –0.033 | 2045 | 1335 | 2865 | 24.0 |
| Minus treatment effect in 2005 | --- | --- | --- | --- | –775 | –125 | 1625 | –9.1 |
| Smoking prevalence (%) | ||||||||
| Men | 52.5 | 32.5 | –20.0 | --- | 1730 | 1488 | 2233 | 20.3 |
| Women | 9.0 | 19.7 | 10.7 | --- | –345 | –260 | –629 | –4.0 |
| Both sexes | 29.7 | 25.8 | –3.9 | --- | 1385 | 1069 | 1604 | 16.3 |
| Total colesterol (mmol/L) | ||||||||
| Men | 5.7 | 5.4 | –0.3 | –0.762 | 2200 | 1485 | 3089 | 25.7 |
| Women | 5.8 | 5.5 | –0.3 | –0.762 | 930 | 615 | 1295 | 10.9 |
| Both sexes | 5.8 | 5.5 | –0.3 | –0.762 | 3130 | 2100 | 4380 | 36.7 |
| Minus treatment effects in 2005 | --- | --- | --- | --- | –480 | –200 | –1005 | –5.6 |
| Body mass index (kg/m2) | ||||||||
| Men | 26.0 | 27.5 | +1.5 | 0.028 | –545 | –304 | –848 | –6.4 |
| Women | 27.4 | 26.7 | –0.7 | 0.028 | 10 | 6 | 17 | 0.2 |
| Both sexes | 26.7 | 27.1 | +0.4 | 0.028 | –535 | –298 | –831 | –6.2 |
| Diabetes prevalence (%) | ||||||||
| Men | 8.3 | 10.5 | +2.2 | --- | –485 | –350 | –631 | –5.7 |
| Women | 10.1 | 9.3 | –0.8 | --- | –155 | –112 | –198 | –1.8 |
| Both sexes | 9.3 | 9.9 | +0.6 | --- | –640 | –460 | –830 | –7.5 |
| Physical Inactivity (%) | ||||||||
| Men | 36.6 | 38.6 | +2.0 | --- | –90 | –72 | –108 | –0.7 |
| Women | 55.7 | 39.2 | –16.5 | --- | 285 | 227 | 340 | 3.3 |
| Both genders | 46.6 | 38.9 | –7.7 | --- | 195 | 155 | 232 | 2.6 |
| Total | --- | --- | --- | --- | 4320 | 3395 | 5205 | 50.6 |
Numbers of deaths prevented or postponed were rounded to nearest 0 or 5.
Additional details of data sources are described in the Supplementary material .
Units are percent change in mortality rate per unit of risk factor as shown in column one
a Results of subtracting the treatments from the best estimate.
Risk factor trends were different in men and women. In men, there were increases in body mass index (1.5kg/m2), diabetes prevalence (2.2%), and physical inactivity (2%). In women, overall diabetes prevalence apparently decreased slightly, paralleling a modest decrease in obesity. More worryingly, an important increase in smoking prevalence (from 9% to 19.7%) was observed in women, adding 345 extra deaths and thus negating some of the gains obtained with the favorable trends in other risk factors.
Sensitivity Analyses: Proportional Contributions to the Fall in Coronary Heart Disease DeathsThe proportional contributions of specific treatments and risk factor changes to the overall fall in CHD deaths in 2005 remained relatively consistent in the sensitivity analyses (Figure 1). Thus, all initial treatments for AMI together accounted for 7.7% of the total 8530 decrease in deaths. The minimum estimated contribution was 4.4% and the maximum was 15.6%. The contribution of AMI treatments therefore remained consistently smaller than that of secondary prevention or heart failure therapies, irrespective of whether best, minimum or maximum estimates were compared (Figure 1).
Figure 1. Sensitivity analysis. The proportional contributions of specific treatments and risk factor changes to the overall decrease in coronary heart disease mortality in Spain between 1988 and 2005. The squares and diamonds show the specific and total best-model estimates, respectively. The vertical lines show the extreme minimum and maximum estimates. AMI, Acute myocardial infarction; BMI, body mass index; BP, blood pressure; CABG, coronary artery bypass grafts surgery; HF, Heart failure; PTCA, percutaneous transluminal coronary angioplasty.
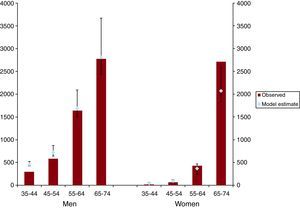
The model estimates also showed reasonable agreement with the observed reduction in CHD deaths across specific age groups in men and women (Figure 2).
Figure 2. Model-estimated and observed reductions in coronary heart disease deaths in Spain between 1988 and 2005. The columns show the observed fall in deaths in each age group; the diamonds show the best model estimates and the vertical lines indicate the extreme minimum and maximum estimates.
DISCUSSIONWe examined CHD trends in Spain, a Mediterranean population where cardiovascular mortality rates are far lower than in Northern Europe or the United States.
CHD mortality rates fell by almost 40% between 1988 and 2005. Approximately half the fall was attributable to evidence-based medical therapies and half to reductions in major risk factors. Even though CHD mortality rates fell substantially between 1988 and 2005 in Spain, the burden of CHD in Spain remains an important public health issue. CHD still accounts for 32% of all deaths21 and also causes substantial disability, long-term dependence on health services and medications, and loss of quality of life.22 Furthermore, CHD is an important factor contributing to stroke occurrence at older ages. In the 17 years of the study there has been rapid growth in costly medical technology and pharmaceutical treatments for CHD, as well as substantial public health efforts to reduce the levels of major cardiovascular risk factors. Establishing the relative contributions of these contrasting approaches is therefore of considerable importance.
This is only the second time that the IMPACT Model has been applied to a Mediterranean country, characterized by substantially lower CHD mortality rates compared with Northern European countries9, 11 and the United States6 given similar levels of the main cardiovascular risk factors in the population (the “Mediterranean paradox”).12 In Italy, we found that age-adjusted CHD mortality rates also fell by approximately 40% among persons aged 25-84 years between 1980 and 2000.12 Approximately 40% of this decrease was attributed to treatments, and approximately 55% to changes in risk factors. Decreases in systolic blood pressure (–5.3mmHg), total cholesterol concentration (–0.35 mmol/L), and smoking prevalence (–4.0%) were estimated to have accounted for approximately 25%, 23%, and 4% of the mortality fall, respectively. Increases in diabetes and body mass index were smaller than in Spain in 2005, resulting in only approximately 2% additional deaths.
Previous studies using the IMPACT methodology in Northern European or United States populations have all consistently shown a greater contribution from reduction in population risk factor levels than from treatments.7, 8, 9, 10, 12In Spain, we found that improvements in major risk factors accounted for approximately 50% of the recent decrease in CHD deaths. The largest mortality benefit came from changes in total cholesterol (about 31% of the mortality fall) and in systolic blood pressure (about 9%). Cholesterol and blood pressure have been steadily decreasing over the past 20 years.4, 23 The decline in systolic blood pressure was more evident in young men than in other groups. Indeed, the proportion of treated hypertension rose to 70% by 2005, although only about 30% were adequately controlled.24 A similar phenomenon could be described with cholesterol: almost 31% of the mortality decrease came from a moderate reduction (0.33 mmol/L) in serum cholesterol level, having separately quantified the effect of statins in primary prevention (barely 1%). Despite an unhealthy diet, other developed countries have also shown decreases in cholesterol levels.25, 26, 27
We found interesting differences in risk factor trends by sex. Although smoking prevalence among men fell from 52.5% to 32.6%, smoking prevalence among women rose distressingly from 9.1% to 19.1%,28 resulting in over 340 additional coronary deaths. In spite of recent declines in smoking prevalence following the workplace smoking ban in Spain in 2006 and 201029, 30 further interventions will clearly be essential.
Furthermore, whereas the body mass index in women apparently decreased from 27.4kg/m2 to 26.7kg/m2, the body mass index rise in men resulted in about 540 additional deaths. Similar results have been described previously in Spain.31 Furthermore, the increase in diabetes prevalence accounted for approximately 640 additional deaths from CHD in 2005.
These adverse trends are depressingly consistent with recent studies in Italy and other Mediterranean countries.12 Stronger interventions are therefore needed in future measures to improve the public health.
As elsewhere, the largest contributions from medical therapies consistently came from secondary prevention, followed by treatment for hypertension, then AMI treatment. Revascularization by coronary artery bypass grafts surgery or coronary angioplasty for stable and unstable disease together accounted for approximately 3.5% of the overall fall in CHD deaths, even less than the 5% in previous studies in the United States and Europe.8, 9, 12, 32, 33 Furthermore, recent trial evidence now suggests that for patients with stable angina, percutaneous transluminal coronary angioplasty provides no mortality benefits compared with optimal medical treatment.8, 9, 12, 32, 33, 34
Modelling studies have a number of potential strengths, including the ability to transparently integrate and simultaneously consider huge amounts of data from many sources, and then test explicit assumptions by sensitivity analyses.
However, all modeling analyses have limitations. Models are dependent on the variable extent and quality of data available. Assumptions have to be made to fill the gaps, and robust sensitivity analysis using the analysis of extremes approach are therefore essential. However, the proportional contributions to the overall reductions in deaths from specific treatments and risk factor changes remained reasonably consistent, irrespective of whether best, minimum, or maximum estimates were considered (Table 2, Table 3). This was reassuring, as was the general consistency with studies performed elsewhere.35, 36
Results from different studies were used to estimate cholesterol level, blood pressure, and body mass index at the beginning and at the end of the study period.4, 24, 37, 38 Variations due to different study designs, study populations, and study periods might therefore influence results. Even though unpublished original data were used together with published sources, publication bias might still be an issue.
Although previous publications have suggested the distribution of prevalence of cardiovascular risk factors may be not homogeneous,39 little variation was observed between Autonomous communities in the population aged 35-74 years in a recent publication.40 The trends in cardiovascular risk factors observed in some areas of Catalonia may also apply to the rest of Spain.
Still more worrisome is the fact that at least 8% of the persons are unaware that they have the disease (undiagnosed or unknown diabetes mellitus).41
The model included only those aged 35-74 years because very limited data was available in older groups. In addition, the model fit was poorer in the oldest women, explaining less of the observed decrease in CHD mortality in this age group compared with men. Elderly women have been shown to be underrepresented in many CHD clinical trials and surveys.42 Furthermore, death certification could be overestimating CHD mortality in elderly groups.
The risk factor estimates clearly remain imprecise. Furthermore, risk estimates were not necessarily fully independent from each other. However, the use of the sensitivity analyses with + 20% thresholds for each parameter, when 95% confidence intervals were not available, helps to give a robust range within which the real value will almost certainly fall. We also did not explicitly consider the effect of lag times; however, they may be relatively unimportant over a 17-year period.9, 11, 43 Although major efforts were made to address overlaps, residual double-counting of some individual patients remains possible. We also assumed that, after adjustments for lower dosing and imperfect compliance, the efficacy of treatments in randomized controlled trials could be generalized to population effectiveness in usual clinical practice.11, 43, 44 Both assumptions may have potentially overestimated the true treatment effect.
We therefore made explicit assumptions detailed in the Supplementary material. Moreover, we only analyzed the estimated fall in CHD deaths, not life years gained or quality of life9. These merit further work, as do economic analyses which would complement the mortality data and help determine priorities when planning future prevention and intervention strategies.
CONCLUSIONSIn conclusion, approximately half of the recent CHD mortality decrease in Spain was attributable to reductions in major risk factors, and half to medical and surgical therapies. Future CHD strategies should therefore actively promote primary prevention and maximize the population coverage of effective treatments.
DISCLAIMERThe findings and conclusions in this article are those of the authors and do not necessarily represent the views of the University of Liverpool or of the Spanish Institutions.
FUNDINGThis work was supported by Spain's Ministry of Science and Innovation through the Carlos III Health Institute and FEDER [Red HERACLES RD06/0009] and the Health Research Fund [CM08/00141 to M.G. and CM06/00212 to G.F.M.]. M.O. was funded by the UK Medical Research Council, and the European Union.
CONFLICTS OF INTERESTNone declared.
Appendix A. Supplementary MATERIALSupplementary material associated with this article can be found, in the online version available, at doi:10.1016/j.rec.2011.05.035.
Appendix A. Supplementary dataReceived 7 January 2011
Accepted 5 May 2011
Corresponding author: Division of Public Health, University of Liverpool, Whelan Building, Quadrangle, Liverpool, L69 3GB, United Kingdom. capewell@liverpool.ac.uk