Keywords
INTRODUCTION
The aims of this study were to investigate left ventricular morphology in a sample of elderly Spanish individuals and to assess differences in this regard between hypertensive and normotensive subjects. The prevalence of cardiac remodeling increases with age, and is estimated to be 43% to 45% among individuals over age 65.1-3 In this group of patients, the prevalence of left ventricular hypertrophy (LVH) is around 15%.1-3 Abnormal left ventricular geometry has been associated with an increased mortality in this patient population4,5 and is higher in patients with hypertrophy.
METHODS
Data for this study were obtained from a patient subgroup of the EPICARDIAN study (EPIdemiología CARDIovascular en los ANcianos, Cardiovascular Epidemiology in the Elderly in Spain). The methodology of the EPICARDIAN study was previously described in detail.6
The sample was randomly selected from among all patients included in the EPICARDIAN study who live in the Salamanca neighborhood of Madrid, Spain. Of the 371 patients who underwent echocardiography, the measurements required for the study could be obtained in 242 (65.2%), whereas in all others, a poor acoustic window precluded proper measurement.
Echocardiography was performed using a Toshiba 160 system with a 2.5-MHz transthoracic transducer. The echocardiography specialists were blinded to the patient's hypertensive or normotensive status, and the degree of agreement was studied to determine the interobserver variability. All echocardiographic measurements were based on the American Society of Echocardiography guidelines published by Sahn et al7 in 1978 in Circulation and were taken in M mode with color Doppler ultrasound. Left ventricular morphology was analyzed by the left ventricular mass index (LVMI), and relative wall thickness (RWT) was obtained by the formula RWT=2´ posterior wall end-diastolic thickness/left ventricular end-diastolic diameter. LVH was considered present when LVMI was >134 g/m2 in men and >110 g/m2 in women, and RWT was deemed normal when ≤0.44. According to these values, patients were classified into 4 types: type I (normal left ventricle: normal LVMI and normal RWT), type II (concentric remodeling: normal LVMI and RWT >0.44), type III (concentric hypertrophy: LVH and RWT >0.44), type IV (eccentric hypertrophy: LVH and RWT ≤0.44). The sample was stratified according to patient sex and age ≥75 and <75 years. Patients who presented atrial fibrillation were excluded from the assessment.
Patients were considered to have a poor acoustic window if any of the following factors could not be measured with certainty in the parasternal long-axis view: end-diastolic diameter, end-systolic diameter, septum, or posterior wall. Patients in whom these measurements were possible were defined as having a good acoustic window. The 2 groups were compared in terms of weight, age, sex, height, body mass index, obesity, hypertension, diabetes, and smoking habits; however, no statistically significant differences were observed.
Statistical Analysis
The categorical variables were described by the distribution frequency, and the continuous variables were expressed as the mean (SD). In order to test the possible association between qualitative variables, we used the c2 or Fisher exact test. Data were processed and analyzed using SPSS, version 10.
RESULTS
The baseline characteristics of the initial sample are shown in Table 1. In all, 291 patients (78.6%) were hypertensive and 80 (21.4%) were normotensive. The mean age of the sample was 74 (6) years. Ejection fraction was 66.4% (9.7%) in normotensive and 70% (11.4%) in hypertensive patients (P<.14). The prevalence of diabetes was 9.2%. The prevalence of a poor acoustic window was 34.4% in the hypertensive group and 36.7% in the normotensive group (P=.7).
Of the 242 patients with a good acoustic window, 191 (78.8%) were hypertensive and 51 (21.4%), normotensive. Distribution by sex was 124 (51.2%) men and 118 (48.8%) women. By age, 152 (62.8%) were <75 years and 90 (37.2%) were ≥75.
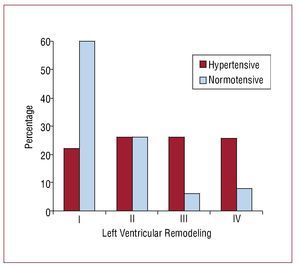
Cardiac remodeling in the 242 patients included was as follows: 74 (30.5%) type I, 62 (25.9%) type II, 53 (21.8%) type III, and 53 (21.8%) type IV. Comparison between hypertensive and normotensive patients (Figure) yielded the following: 42 (22.3%) type I, 50 (26.1%) type II, 50 (26.1%) type III, and 49 (25.5%) type IV in hypertensive patients and 31 (60%) type I, 13 (26%) type II, 3 (6%) type III, and 4 (8%) type IV in normotensive ones (P<.0005).
Figure. Left ventricular remodeling. Comparison between hypertensive and normotensive patients.
The sample was stratified according to sex and age. Cardiac remodeling was observed in men as follows: 43 (34.1%) with type I, 31 (25.2%) with type II, 27 (22%) with type III, and 23 (18.7%) with type IV; and among women, 32 (26.7%) type I, 32 (26.7%) type II, 25 (21.6%) type III, and 29 (25%) type IV (P=.5).
In terms of age, patients younger than age 75 showed the following: 54 (35.6%) with type I, 35 (22.6%) with type II, 30 (19.9%) with type III, and 33 (21.9%) with type IV; among those age 75 or older: 21 (22.6%) type I, 28 (31.2%) type II, 22 (24.7%) type III, and 19 (21.5%) type IV (P=.14).
DISCUSSION
The results of this study show a lower overall prevalence of ventricular remodeling without LVH compared with previous studies,8,9 whereas the prevalence of LVH was similar. This difference may be due to methodological aspects or to the fact that our study did not include history of ischemic heart disease in the analysis.
The prevalence of cardiac remodeling in the overall population was similar when the sample was stratified by sex and age, and any differences were statistically insignificant. These results are similar to those reported in other series.8,9
In addition, the comparison between hypertensive and normotensive patients showed a higher percentage of morphologic abnormalities in those with hypertension. The probability of normal morphology in older hypertensive patients was 1 out of 5, data similar to those observed in previous studies.8,9
Limitations
The sample was recruited from the general population census of an area in Madrid with a high socioeconomic level,6 which could explain the low overall incidence of atrial fibrillation compared to other published series. Moreover, the history of ischemic heart disease was not analyzed. These considerations could lead to a lower statistical value.
This study was carried out with funds from the Fondo de Investigaciones Sanitarias (Health Research Fund), Files 93/0012-02, 96/1993-01, 970197, and 02/0896.
Correspondence: Dra. C. Suárez.
Servicio de Medicina Interna. Hospital Universitario de La Princesa. Diego de León, 62. 28006 Madrid. España.
E-mail: csuarez.hlpr@salud.madrid.org
Received April 15, 2009.
Accepted for publication August 25, 2009.