Keywords
INTRODUCTION
Remote magnetic navigation using the Stereotaxis® system (STX) is a new approach to the ablation of arrhythmias. It avoids exposing the operator to radiation energy when handling the ablation catheter, since this can be done at some distance from the patient. By means of a system of large magnets situated on both sides of the patient, the STX system can be used to remotely guide the ablation catheter tip, manually or automatically. It has been suggested that the STX system may provide increased catheter stability.1,2
The STX system has already been used for mapping and ablation in most arrhythmia contexts, with success rates similar to conventional ablation techniques.1-5
Given that the magnetic field helps to maintain the catheter on the target area with theoretically increased stability, the aim of the study was to assess whether improved tissue contact necessitates a change in conventional radiofrequency (RF) ablation parameters. To simplify the situation regarding the anatomical substrates, we only focus on the ablation of atrioventricular nodal reentry tachycardia (AVNRT) in the slow pathway in the inferior paraseptal region of the right atrium. Thus, we report our initial experience in the AVNRT ablation in the first 19 consecutive patients treated with the STX system using 4-mm catheters and compare them to a recent registry of 18 patients who underwent ablation using conventional 4-mm catheters. The study compared the RF energy parameters needed to ensure that AVNRT could not be induced (maximum, 1 nodal echo beat) in both groups after ablation.
METHODS
Study Population
All patients were referred for electrophysiological study (EPS) and ablation for symptomatic paroxysmal supraventricular tachycardia. A total of 37 patients who underwent ablation for common AVNRT or its variants were included. Patients who had previously been treated with ablation for recurrence were not included. Of the 37 patients, 19 had been treated using the STX system since September 2007, and were the first consecutive patients in Spain treated with this technique. The control group consisted of the remaining 18 patients who were treated using a conventional approach. Of these, 13 were the last consecutive patients to undergo ablation using the conventional technique in the months preceding setting up the STX control room. The remaining 5 consecutive patients were treated for AVNRT in subsequent months, but without the STX system, since the STX control room was not available on the day the patients were scheduled for study and ablation. This was due to reasons unrelated to the patient (control room inspection or its use as a cardiac catheterization laboratory).
Electrophysiological Study
After giving informed consent for AVNRT ablation, the patients underwent EPS in a fasting state and without antiarrhythmias for at least 5 half-lives, as performed conventionally.6 Three diagnostic 4-pole catheters (5-6 Fr) were introduced via the right femoral venous route to be positioned in the right atrium, the bundle of His region, and the right ventricle for the diagnostic EPS. In cases in which baseline EPS could not induce AVNRT, isoproterenol was used in progressive doses for induction and to verify the endpoint (Table 1).
After electrophysiological diagnosis of AVNRT, in patients receiving conventional treatment, the ventricular catheter was exchanged for a 4-mm ablation catheter (Marinr MCXL, Medtronic or Celsius F, Biosense-Webster) in order to proceed with the ablation. In patients treated with the STX system, the ventricular catheter and its introducer sheath were removed and replaced by an SR0 sheath (St Jude Medical, St Paul, Minn., USA ), and this was introduced up to 1-2 cm below the junction of the right atrium and inferior vena cava. This was used to guide a 4-mm STX ablation catheter (Celsius RMT or NaviStar RMT, Biosense-Webster) to the region of the His bundle. The use of the sheath with the STX system was recommended by the STX technical staff, who pointed out that given the high flexibility of the catheter it would not reach the right atrium without support.
Remote Navigation System
The STX Remote Magnetic Navigation system (Niobe, Stereotaxis) consists of 2 permanent computer-controlled magnets, positioned on either side of the patient's torso, that allow a magnetic-tip catheter to be remotely steered into the cardiac cavities. The 2 magnets create a magnetic field of approximately 15 cm (0.08 T) that can be modified by the operator to steer the catheter tip in the desired direction. The system has a small motor drive unit (Cardiodrive unit, Stereotaxis®) coupled to the catheter allowing it to be advanced or withdrawn, which allows remote navigation while reducing the fluoroscopic exposure time for the operator.2
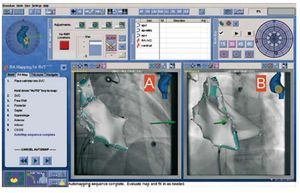
To aid intracardiac navigation, the STX system is integrated with the Carto® electromagnetic mapping unit and automatically creates 3D maps of the target cavity via the automated movement of the explorer catheter itself (Figure 1). This system was used in 3 patients. Furthermore, without requiring the use of the Carto system, the incorporation of the fluoroscopy unit with the STX system enables defining target areas with the STX workstation (Navigant®, Stereotaxis), such as the location of the His bundle or the coronary sinus, and that will appear from that moment onward on the fluoroscopy monitor in real-time to help locate the anatomical position of the ablation catheter at all times (Figure 2). This approach was used in the remaining 16 patients.
Figure 1.The remote control system console. The 2 lower panels (A and B) show the right atrium automatically reconstructed by the magnetic navigation system. The reconstructed cavity is shown as a 3D image (Carto® system) incorporated in the fluoroscopic image in the RAO view (A) and LAO view (B). The green arrows indicate the current direction of the explorer catheter.
Figure 2. The remote navigation system console without the associated Carto® system. The 2 upper panels (A and B) show the virtual icon used to adjust the navigation vectors in 3D and that can also be done from the three side panels. The lower panels (C, RAO; D, LAO) show the fluoroscopic images where, after local manual mapping, the 3 key points of the triangle of Koch have been marked: the His bundle, the ostium of the coronary sinus (SCo) and paraseptal attachment of the tricuspid valve (AT). The effective point of RF application is also marked in red.
Ablation
The conventional criteria for slow pathway ablation-modification were followed by anatomical and electrophysiological criteria. The aim of ablation was modification of the slow pathway until it was ensured that no type of AVNRT could be induced (maximum, 1 nodal echo beat) in baseline conditions or after the administration of isoproterenol if this was required for induction.
In the STX group, ablation was performed using a Stockert RF generator (Biosense-Webster) in temperature controlled mode (maximum temperature, 50oC; maximum power, 40 W) in 18 of the 19 patients. In the control group, the Stockert generator was used in 15 patients and the Atakr II generator (Medtronic) in 3 patients, both in temperature control mode. The RF current parameters were adjusted to a maximum temperature of 60-65oC and a maximum power of 50 W in all cases, as is conventional in our hospital. The following were recorded during each application of RF energy: application time, mean temperature reached, total energy delivered (once stabilized after the first few seconds), and the mean impedance values obtained during the application. Based on these registries, we calculated the total number of applications per patient, the number of applications ≤5 s and the maximum, minimum and average values of temperature, power and impedance attained. The range of temperatures and impedances obtained were calculated as the difference between the maximum and minimum value for temperature or impedance recorded during the different applications in the same case. We measured the total RF energy delivered (J) as the sum of mean power delivered for the duration (s) of application for each application. The ablation catheter tip was examined to rule out charring if unusually low powers were recorded and at the end of the procedure.
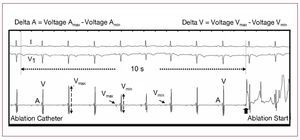
To compare the stability of the STX catheter intracavitary electrical recordings with conventional recordings, we analyzed beat-to-beat variability and that linked to breathing in the local electrograms recorded at the distal dipole of the ablation catheter. Thus, the ablation catheter endocavitary signal was analyzed for variations in voltages of the atrial (A) and ventricular (V) electrograms during the 10 s prior to the first two applications of RF energy in each patient (Figure 3). DA was defined as the difference between the maximum and minimum voltage recorded in the atrial electrograms during the 10-s period referred to. DV was defined in the same way for the ventricular electrograms. Theoretically poor positions, due to poor catheter-tissue contact, should lead to higher values of both D.
Figure 3.Example of analysis of the endocavitary signal of the ablation catheter showing variations in voltage of the atrial (A) and ventricular (V) electrograms during the 10 s prior to the first RF application of a patient treated using the STX system. Delta A is defined as the difference between the highest and lowest voltage recorded in the atrial electrograms during these 10 s. Delta V is similarly defined for the ventricular electrograms. The normal variations in voltage especially characteristic of cardiac movement during breathing can be observed.
On the other hand, with the aim of documenting whether the applications were performed using similar electrical and anatomical criteria in the STX and control groups, we decided to analyze the atrial and ventricular electrograms of the 5 beats immediately before each of the first 2 applications of RF energy in each patient (this was always done in the lower paraseptal region for increased safety). A priori, significant differences in the A/V ratio (average voltage quotient of the 5 atrial and ventricular electrograms) would indicate that it had not been applied to the same region or at least using the same criteria, either because of predominance of a ventricular signal in one of the series, due to more ventricular applications, or because of atrial predominance in the atrial positions.
We decided to only compare the first 2 applications because, under normal circumstances, the subsequent ones can involve more atrial applications or higher ones (positions involving greater risk) if AVNRT is still inducible or more than 1 nodal echo beat persists. This would render meaningless the comparison of averages of all the applications of all the patients due to potentially very different A/V ratios in each patient and between patients. Similarly, we quantified the onset of junctional rhythms during applications in both groups, as their presence indicates that it is actually being applied on the nodal tissue. We recorded the number of patients who presented some type of nodal rhythm (NR), its minimum cycle-length (the most rapid NR) and maximum cycle-length (slowest), the sum of all nodal beats of induced NR, the sum of the total duration of all the induced NR, as well as the average time between the beginning of RF energy application and the onset of the next NR in all applications that were followed by the NR in each patient.
The following were quantified: total procedure time, fluoroscopy times, the radiation energy dosage measured by the dose-area product (DAP) quantified by the x-ray apparatus itself in Gy/cm2 and the number of cine runs per patient.
Statistical Analysis
Continuous variables with a normal distribution were expressed as mean (SD) and those with a non-normal distribution were expressed as average (semiquartile range). Continuous variables were analysed for normality using the Kolmogorov-Smirnov test with the Lilliefors correction. Continuous variables were compared using the Student t test for unmatched samples or the Mann-Whitney U test if appropriate. Discrete variables (sex of the patients, proportion of 5-s applications, type of AVNRT, use of isoproterenol, onset of nodal rhythm and the analysis of recurrence) were compared using the Fisher exact test. The differences were considered statistically significant if the null hypothesis could be rejected at a confidence level greater than 95%. All calculations were performed using the SPSS version 15.0 application (SPSS, Chicago, Illinois, USA).
RESULTS
Characteristics of the Patients and Ablation
There were no significant differences between the two groups regarding the age and sex of the 36 patients. The 19 patients treated using the STX system had a mean age of 55 (21) years; 12 of them were women. The type of induced tachycardia and the use of isoproterenol are shown in Table 1.
Conventional parameters were employed for AVNRT ablation (65oC; 50 W) in the first patient treated with the STX system. After the first applications clear charring was observed in almost the entire tip. The impedance recorded during its application decreased from an initial 160-165 W to 120-130 W; subsequently, there was an isolated peak of 285 W. Similarly, a decrease of delivered power from 50 W to 10 W was observed for a target temperature (65oC).
Thus, we reduced the energy in all other cases of STX to a maximum temperature of 50oC and a maximum power of 40 W, following the recommendations of the STX technicians. For the analysis of results, we only included these 18 patients who received homogeneous treatment. In all cases of ablation using the STX system, patient tolerance was excellent and there were no cases of adverse events or complications.
In the control group, the mean age of the 18 patients was 52 (14) years; this group included 12 women. The Marinr® catheter was used in 15 patients in this group and the Celsius® in 3. No charring or noteworthy adverse events were recorded at the programmed temperatures and powers (60-65oC; 50 W).
In the 36 patients, no type of AVNRT could be induced after ablation nor was there more than one nodal echo beat.
Table 1 shows the comparison between the two groups of induced nodal rhythms after applying RF energy to the perinodal region. There were no significant differences in the total number of patients who presented them nor in the characteristics of the nodal rhythms regarding cycle length, number of beats or their duration. There was a trend toward a shorter period between the beginning of applications and the onset of nodal rhythm in the control group.
Applied Radiofrequency Energy
There were no significant differences between the STX group (6 [11]) and the control group (9 [9]; nonsignificant differences) (Table 2) in the total number of applications needed to achieve successful ablation. Neither were any differences recorded in the total duration of RF energy application between the two groups (STX, 114 [171] s; control, 114 [65] s; nonsignificant differences).
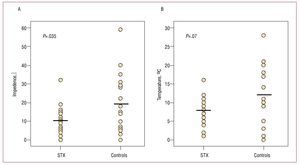
However, the temperature reached and the mean power delivered were significantly lower in the STX group (Figure 4A and 4B). Thus, the mean temperature reached was 46 (2) oC in the STX group versus 50 (4) oC in the control group (P<.001) and the average actual power delivered was 29 [14] W in the STX group and 50 [7] W in the control group (P<.001); no charring occurred in either of the 2 groups. However, no significant differences were found in total energy delivered between the STX group (3228 [6052] J) and the control group (5447 [4893] J; nonsignificant differences) (Figure 4C).
Figure 4.Radiofrequency energy parameters achieved during ablation in the stereotaxis (STX) and control groups after initial adjustment of the ablation parameters to maximum temperatures and powers of 50oC/40 W and 60-65oC/50 W, respectively. A: comparison of the temperature reached, averaging all RF applications in each case in the STX group and the control group. B: average values of power delivered between the 2 groups. C: final RF energy delivered in the two groups. The horizontal bars in the 3 panels indicate the average values.
Three different operators performed the procedures, one of whom performed the greatest number of procedures: 16 control patients and 11 STX patients. If the results obtained by this operator are analysed in isolation, the results are similar to those described in the total series regarding temperature (P=.001), mean power (P<.001), and energy (P=.4). No significant differences were found in the ablation parameters recorded between the first 9 patients in the STX group and the last 9 in the same group.
Stability
Good local stability was obtained during ablation in the STX group, despite the minimum robustness of the ablation catheter. Analysis of the electrograms recorded at the distal dipole of the remote catheter did not indicate significant differences when compared to the conventional catheters used in the control group (Table 3). Similar atrial and ventricular voltages and A/V ratios were found in both groups, with no significant differences in variations of voltage due to breathing or the cardiac cycle, as shown by analyzing the electrograms of the 10 s prior to the first two applications. The maximum values of DA correspond to 2 isolated cases, one in each group, where the voltage of the first beats of the 10-s band was much greater than that of the 5 last beats, just before application. In a conventional protocol of applications to the slow pathway, such as the one we followed and which avoids high-risk applications, many applications ≤5 s tend to occur because of catheter displacement just after starting to apply RF energy. We analyzed the distribution in both groups. Only in 4 patients in the STX group were there applications ≤5 s vs 11 patients in the control group (P=.041).
The impedances recorded during the RF energy applications were also recorded. No significant differences were found in the average value of all the impedances recorded per case between the STX group (mean, 150 [13] W) and the control group (144 [16] W; nonsignificant differences). However, there was a significantly smaller variation in the range of impedances obtained during application (maximum impedance recorded minus the minimum impedance of all applications in each case) in the STX group than in the control group (10.4 [7.6] vs 19.3 [15.4] W; P=.035, respectively) (Figure 5A). Regarding the variations of temperature between different applications in each patient, there was a tendency toward smaller variations in mean temperature in the STX group (STX, 7.9 [3.6] oC vs control, 11.8 [8.2] oC; P=.07) (Figure 5B). These values indicate more homogeneous and stable contact between different applications during ablation. If the data obtained by the main operator involved in the study are analyzed in isolation, similar results are found in the average value of impedance (nonsignificant differences), range of impedances (P=.002), and range of temperatures (P=.046).
Figure. 5.Range of impedances (A) and temperatures (B) reached during ablation between applications, showing the highest and lowest values in the stereotaxis (STX) and control groups. The horizontal bars in panels A and B indicate the mean values. Smaller variations can be observed in the STX group, which indicates a more stable and homogeneous contact between applications.
Procedure Times and Radiofrequency Dosage
Table 4 shows the descriptive statistics of the procedure time, total fluoroscopy time, radiation dosage and number of cine runs. Despite including the first cases of the STX group, the STX procedure times were on average 17% longer than the control group (nonsignificant). There were no significant differences in total fluoroscopy time. However, the total radiation dosage was clearly greater in the STX group, since more cine runs were performed to better document the STX group, including remote movement of the catheter, for educational purposes due to the novelty of the technique.
Follow-up
No late complications were recorded in any of the 37 patients. All the patients were reviewed 6 months after the procedure by protocol. Only one of the patients treated in the control group presented AVNRT recurrence. The patient underwent a second procedure, which was successful and without adverse events. A single recurrence in 37 patients is insufficient to show significant differences in efficacy between the 2 techniques (Fisher exact test, P=.49).
DISCUSSION
We report our initial experience and first results of ablation using a remote magnetic navigation system in Spain. Focusing on AVNRT ablation, we demonstrate that in our series this was safe and without complications after initial readjustment of the ablation parameters. No complications were recorded in an a priori dangerous physical substrate, such as proximity to the AV node, or due to the fact that the study was conducted during the STX system training period. In the present series, conventional RF energy parameters led to just one case of obvious charring during the first applications. This involved a high degree of superficial harmful necrosis due to temperatures >100oC between the endocardium and catheter. The reduction of these parameters to more conservative levels led to the same immediate and long-term success rates as conventional parameters, without requiring increases in the number of applications or their duration.
Efficacy and Security
Our results are in line with previous studies on conventional AVNRT ablation7 and those using remote systems.1,2,8 In a series of 42 patients, Ernst et al2 reported that remote ablation is effective and safe, since there were no complications in any of the ablation procedures. This study highlighted the advantages of remote navigation for patient and physician safety. Thus, in the first group, it is noteworthy that no cardiac perforation occurred using this technique, anatomical stability was high even during tachycardia and there was the potential to return to a site almost automatically. For the operator, the main advantage is performing ablation in a room away from the patient, without radiation energy exposure.2
Similar results have been reported on the efficacy and safety of intranodal ablation in smaller series,1,8 although in one of these initial series8 1 case of transient 2:1 AV block was described.
Radiofrequency Energy and Stability Parameters
Due to the charring recorded in the first patient, we reduced the target temperature and maximum power, both by 20%, obtaining the same effectiveness as in the control group and without the need for more or longer applications. It is noteworthy that similar results were obtained despite these reductions. The success of ablation using lower mean temperatures in the remote group was also described by Davis et al1 despite programming identical RF energy parameters in both groups and using a single RF energy source and a control catheter similar to the remote catheter.
Studies on remote navigation have used different parameters. Ernst et al2 applied RF energy using a target temperature of 55oC at a maximum power of 40 W, which was relatively similar to our settings, and achieved noninducibility with a similar number of applications to ours. However, Kerzner et al8 programmed up to 50 W, although they do report whether charring occurred, and Davies et al1 programmed a target temperature of 50oC and a maximum power of 30 W. Given these differences reported in the literature, and after assessing the recommendations of the manufacturers of the Stereotaxis system, we decide to apply a maximum of 40 W. Our results indicated that, when adjusting the temperature in the remote group to 50oC, the average of mean power finally applied was 29 W, with a mean power <37 W in 75% of cases, and delivering a power of <37 W only in 10% of patients in the control group. The delivered power is relevant, since this is what finally determines the size of the lesion9; the lower the power, the smaller the lesion size. Given the relevance of the area treated in AVNRT—the nodal slow pathway in the areas near the AV node— it is desirable to obtain noninducible tachycardia with the least volume of necrosed tissue.
The charring that occurred in the first patient treated with the remote guidance system (RF energy set at 65oC, 50 W), is the first we have observed in more than 400 AVNRT ablations. This could be due to having strong support at their tips, which may lead to very high temperatures being reached (>100oC when charring) despite blood flow acting as a local heat-sink.10 After reducing these parameters, no charring occurred in any of the 18 remaining patients.
In a study similar to ours, but performing circumferential ablation of atrial fibrillation, Di Biase et al10 recently reported a high rate of charring in 4-mm remote catheters during which powers of up to 50 W were also applied. After this finding they reduced the maximum power to 40 W, but continued to find charring in up to in a third of the cases when conducting ablation for atrial fibrillation, a situation that was clearly different from ours. The absence of new charrings in our series when delivering 40 W may have been due to greater blood flow acting as a heat-sink in the peritricuspid region compared to areas such as the posterior wall of the left atrium.
The increased stability of remote catheters has been noted since the first studies on this system were published.2 In the case of AVNRT ablation, stability during each application was the same as that in the series of Davis et al,1 because there was less variation in the range of temperatures during each application with the remote catheter. We analyzed the variability between the different RF applications and obtained similar results, which also indicates a greater homogeneity of contact between applications. Similarly, there were fewer applications ≤5 s with the remote system, many of which were interrupted due to catheter displacement just after beginning the application. This result was also found in the series of Kerzner et al.8 However, in our series the trend toward nodal rhythm onset occurring in the control group before that in the STX group could be a confounding factor.
Limitations
It should be emphasized that the patients in the present study were treated during the training period of the Stereotaxis system in our center. On the other hand, the relatively small number of patients included may explain the wide interquartile ranges of some of the analyzed parameters. Another limitation of the study is that our conventional AVNRT ablation group was compared to a control group that included patients treated with 2 different control catheters and 2 RF energy sources, as routinely carried out in our center. We cannot rule out that some of the differences in impedance may have been due to these two factors. The use of a sheath (a very long introducer) only in the ablations performed using the remote system could be seen as the source of stability. The end of the sheath remained in the junction between the inferior vena cava and right atrium, 4-5 cm below the catheter tip. However, if it were not for the magnetic field, the enormous flexibility of the catheter would lead to it spontaneously bending (180o) at this point (4-5 cm) which would eliminate any relevant stability provided by a scabbard. Finally, we believe it unlikely that the use of the navigator in 3 of the patients in the STX group was an obvious factor regarding heterogeneity when comparing of our series of 37 cases. In this series, the ablation parameters were not modified nor were there a significantly greater or lower number of applications than in other patients in the STX group (all the values within the 25th and 75th percentiles of the remaining STX group).
CONCLUSIONS
In our initial series of patients who underwent AVNRT ablation by remote magnetic navigation, we achieved a level of efficacy similar to that obtained using the conventional manual technique while using 20% less RF energy and with fewer involuntary catheter displacements. In the only case in which we used greater power (50 W) obvious charring occurred which was probably due to more homogenous catheter-tissue contact. A larger randomized clinical study and an experimental study are needed to demonstrate if potential better remote catheter-tissue contact is the definite cause of charring using the conventional 50 W and if identical clinical results can be achieved with less total energy than with the greater typical energies used in the standard manual technique.
ABBREVIATIONS
AVNRT: atrioventricular nodal reentry tachycardia
EPS: electrophysiological
IQR: interquartile range
SD: standard deviation
STX: Stereotaxis
Correspondence: Dr. J. Moreno.
Unidad de Arritmias (2.a Norte). Instituto Cardiovascular. Hospital Clínico San Carlos.
Prof. Martín Lagos, s/n. 28040 Madrid. España.
E-mail: jmoreno@secardiologia.es
Received September 15, 2008.
Accepted for publication June 10, 2009.